Constipation is common and may be due to a variety of causes. Constipation is generally defined as bowel movement frequency < 3 times per week. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who are constipated often strain to pass hard stools. The condition is classified as primary (also known as idiopathic Idiopathic Dermatomyositis or functional constipation Functional Constipation Pediatric Constipation) or secondary, and as acute or chronic. Primary/ functional constipation Functional Constipation Pediatric Constipation can be divided into normal transit, slow transit, and outlet constipation. Constipation is a symptom, not a disease, and appropriate management requires an evaluation of possible etiologies, such as systemic disorders and drugs. Once secondary causes have been eliminated, idiopathic Idiopathic Dermatomyositis constipation can be managed with lifestyle modifications and medications.
Last updated: May 17, 2024
Constipation is a symptom generally defined as bowel movements < 3 times per week; stools are frequently difficult to pass.
Constipation can be classified as either primary or secondary, as well as by duration (acute or chronic).
Primary constipation, also known as functional constipation Functional Constipation Pediatric Constipation, is when there are no identifiable medical disorders. Primary constipation may be due to:
Secondary constipation is constipation due to a medical disorder or medication.
| Etiology | Examples |
|---|---|
| Structural causes |
|
| Endocrine and metabolic disorders |
|
| Neurologic disorders |
|
| Psychiatric disorders |
|
| Connective tissue Connective tissue Connective tissues originate from embryonic mesenchyme and are present throughout the body except inside the brain and spinal cord. The main function of connective tissues is to provide structural support to organs. Connective tissues consist of cells and an extracellular matrix. Connective Tissue: Histology disorders |
|
| Medications |
|
The pathophysiology of constipation varies depending on the etiology, but in general, there are 2 primary mechanisms that cause constipation: altered stool consistency Consistency Dermatologic Examination and altered bowel motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility.
Altered bowel motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility leads to ineffective peristalsis Peristalsis A movement, caused by sequential muscle contraction, that pushes the contents of the intestines or other tubular organs in one direction. Gastrointestinal Motility and difficulty passing stool regardless of its consistency Consistency Dermatologic Examination, leading to sensations of incomplete and irregular bowel emptying. Altered bowel motility Motility The motor activity of the gastrointestinal tract. Gastrointestinal Motility may arise from a number of mechanisms, including:
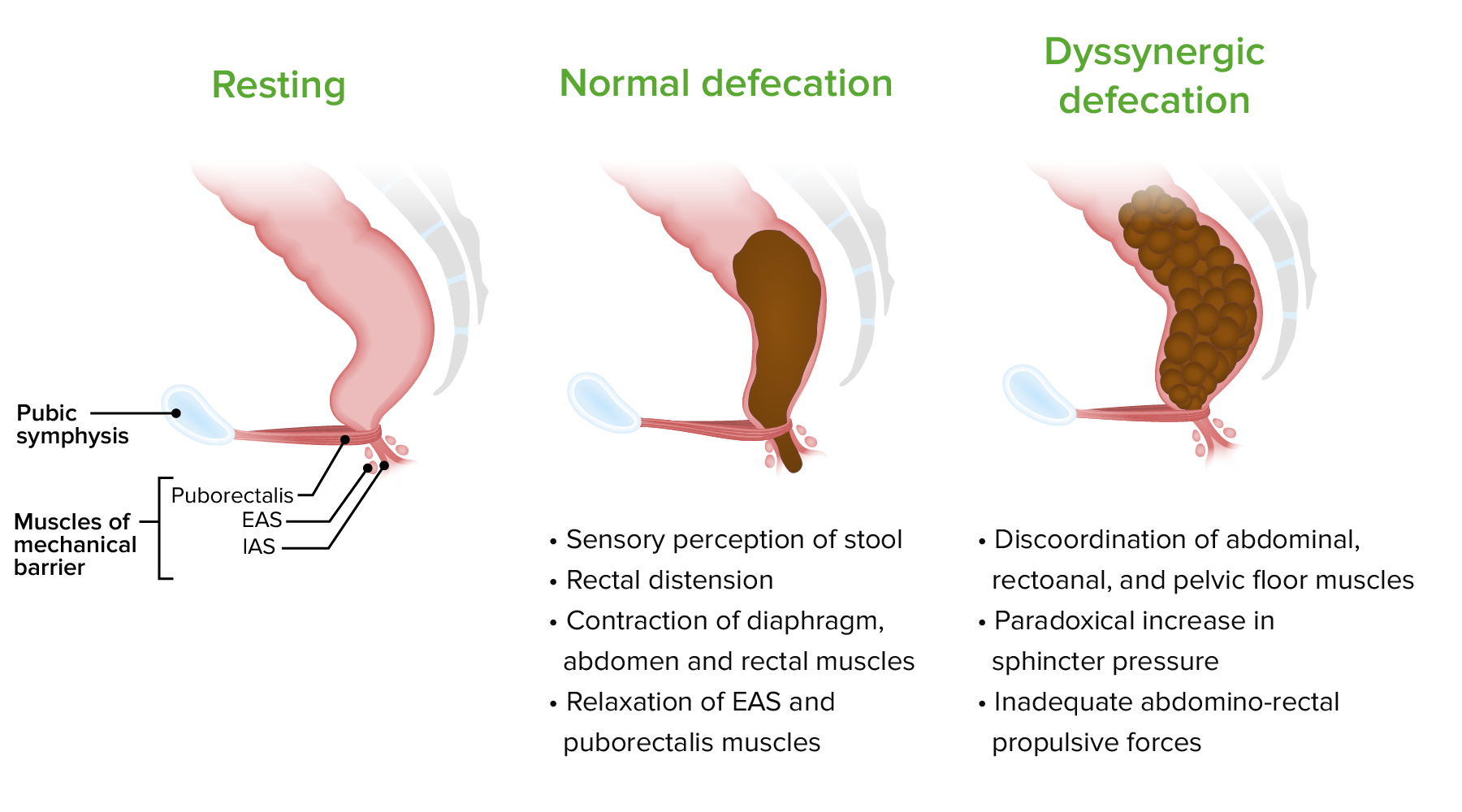
Pathophysiology of dyssynergic defecation:
EAS: external anal sphincter
IAS: internal anal sphincter
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may be asymptomatic, or they may present with the following symptoms:
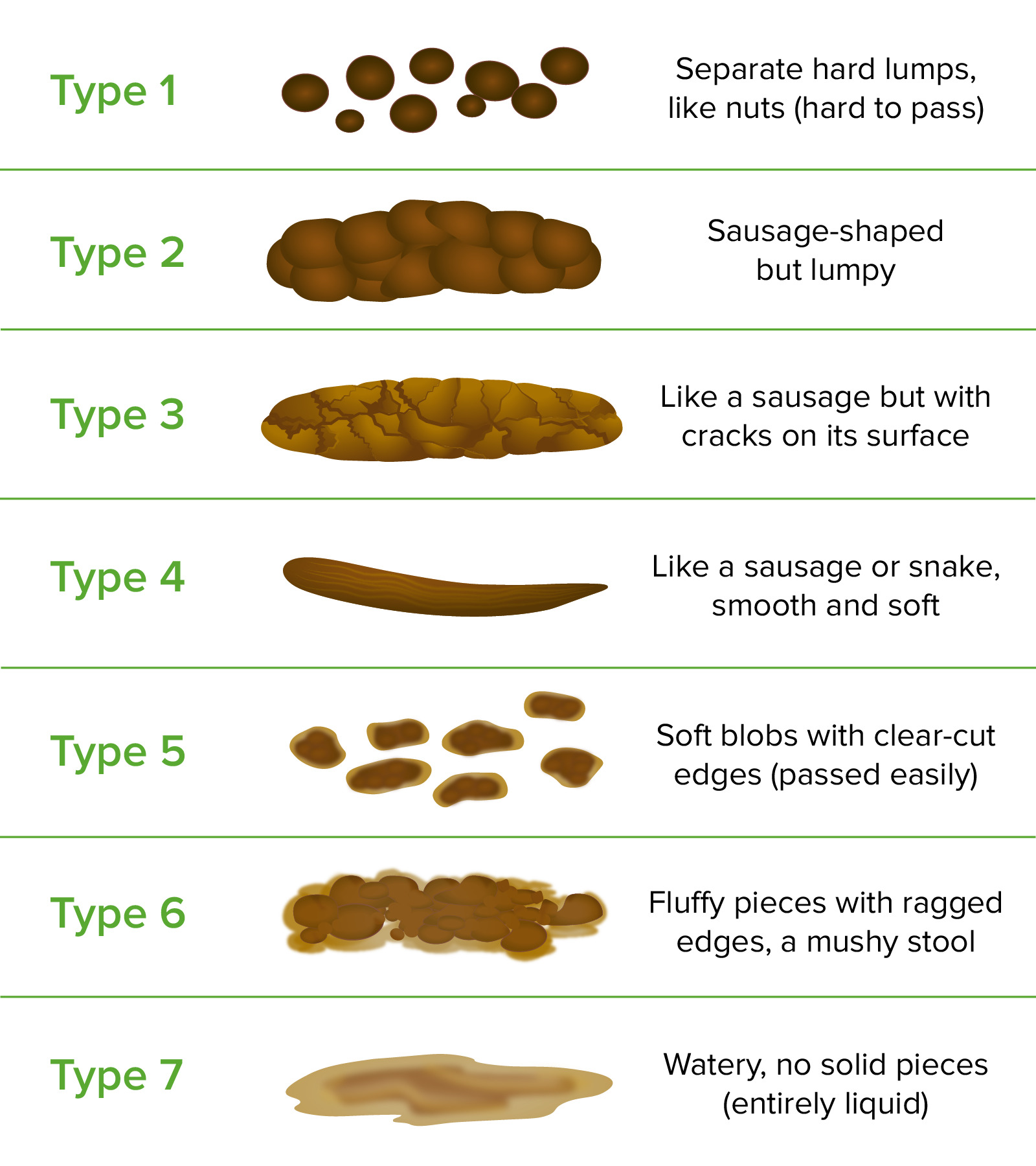
The Bristol Stool Scale
Image by Lecturio.
Hemorrhoids
Image: “M 44 anus 22” by Pachacamac33. License: Public DomainConstipation is a clinical diagnosis. The Rome IV diagnostic criteria for functional constipation Functional Constipation Pediatric Constipation are used in cases with normal transit time.
Criteria:
At least 2 of the following must have occurred in ≥ 25% of defecations during the past 3 months, with the onset of symptoms ≥ 6 months ago:
Indications:
Indications for further workup include:

Measurement of colonic transit time based on radiopaque markers in a patient with chronic idiopathic constipation:
The plain abdominal X-ray is divided into three segments and the radiopaque markers in each segment are counted.
The 1st step in management should be to identify and treat any causes of secondary constipation. Next, management should focus on lifestyle changes and use of bulk-forming agents, followed by osmotic laxatives Osmotic Laxatives Laxatives, adding surface-acting agents, and finally using stimulant laxatives Stimulant Laxatives Laxatives.
If initial management is inadequate, additional options are available, including:
| Class | Mechanism | Indications | Examples |
|---|---|---|---|
| Suppositories Suppositories Medicated dosage forms that are designed to be inserted into the rectal, vaginal, or urethral orifice of the body for absorption. Generally, the active ingredients are packaged in dosage forms containing fatty bases such as cocoa butter, hydrogenated oil, or glycerogelatin that are solid at room temperature but melt or dissolve at body temperature. Large Bowel Obstruction | Liquifies stool | Defecatory dysfunction and/or obstruction | |
| Enemas and lubricants | Soften stool and provide lubrication | Fecal impaction or acute constipation |
|
| Bulk-forming agents | Retain water within the stool and increase fecal mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast | Mild to moderate constipation; best option for long-term management |
|
| Osmotic agents | Poorly absorbed sugars remain in the lumen and lead to water retention in the stool | Chronic idiopathic Idiopathic Dermatomyositis constipation with inadequate response to lifestyle changes and bulk-forming agents (effective in 2‒3 days) |
|
| Surface-agents | Lower the surface tension Surface tension The force acting on the surface of a liquid, tending to minimize the area of the surface. Acute Respiratory Distress Syndrome (ARDS) of stool leading to increased water and fat within stool | Short-term prophylaxis Prophylaxis Cephalosporins (e.g., postoperative care Postoperative care After any procedure performed in the operating room, all patients must undergo close observation at least in the recovery room. After larger procedures and for patients who require hospitalization, observation must continue on the surgical ward. The primary intent of this practice is the early detection of postoperative complications. Postoperative Care) | |
| Stimulant laxatives Stimulant Laxatives Laxatives | Alter electrolyte transport of the intestinal mucosa Intestinal Mucosa Lining of the intestines, consisting of an inner epithelium, a middle lamina propria, and an outer muscularis mucosae. In the small intestine, the mucosa is characterized by a series of folds and abundance of absorptive cells (enterocytes) with microvilli. Small Intestine: Anatomy and increase intestinal motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology activity | Severe constipation not controlled with other treatments (effective in 24 hours) | |
| Chloride Chloride Inorganic compounds derived from hydrochloric acid that contain the Cl- ion. Electrolytes channel activators | Leads to water and chloride Chloride Inorganic compounds derived from hydrochloric acid that contain the Cl- ion. Electrolytes secretion Secretion Coagulation Studies into the stool | Opioid-induced constipation |
|
| Prokinetics | Serotonin Serotonin A biochemical messenger and regulator, synthesized from the essential amino acid l-tryptophan. In humans it is found primarily in the central nervous system, gastrointestinal tract, and blood platelets. Serotonin mediates several important physiological functions including neurotransmission, gastrointestinal motility, hemostasis, and cardiovascular integrity. Receptors and Neurotransmitters of the CNS 5-HT4 receptor Receptor Receptors are proteins located either on the surface of or within a cell that can bind to signaling molecules known as ligands (e.g., hormones) and cause some type of response within the cell. Receptors agonists | For severe constipation in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship ≥ 65 years old, not controlled with other treatments |
|
| GC-C agonists | Induces cGMP cGMP Guanosine cyclic 3. Phosphodiesterase Inhibitors, which leads to increased water and electrolyte secretion Secretion Coagulation Studies into the lumen |
|
|
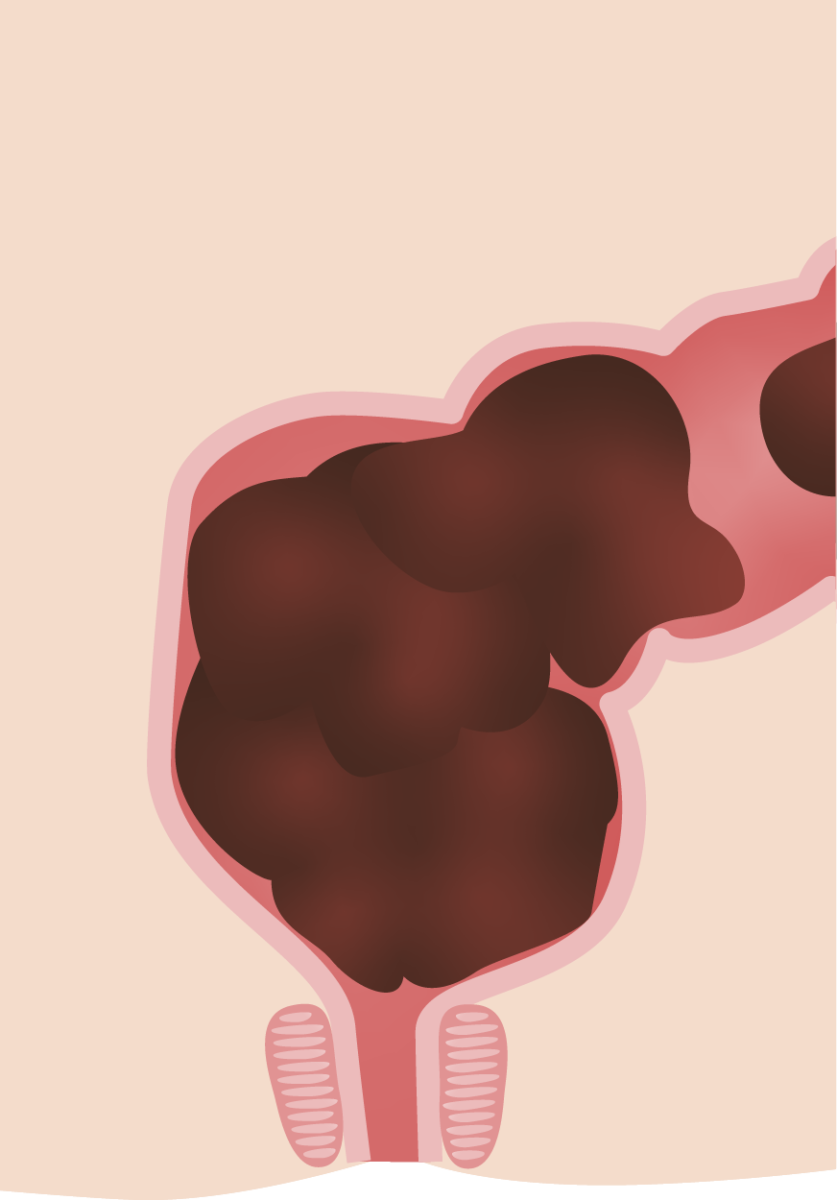
Cross section of the rectal vault in constipation:
This large fecal burden is often seen in functional constipation in children.