Osteogenesis imperfecta (OI), ou "doença dos ossos frágeis", é uma doença genética rara do tecido conjuntivo caracterizada por uma fragilidade óssea grave. Embora a OI seja considerada uma única doença, inclui mais de 16 genótipos e fenótipos clínicos com diferentes graus de gravidade dos sintomas. Destes 16, os tipos I-IV são os mais comuns. Devido à raridade da OI, esta é considerada uma "doença órfã" nos Estados Unidos. O diagnóstico é feito clinicamente, através da história e do exame objetivo, e é confirmado com achados imagiológicos e análise do DNA. Embora não haja uma cura definitiva, o tratamento é de suporte, geralmente envolvendo bisfosfonatos, e foca-se na redução da dor, redução da frequência de fraturas, redução da deformidade óssea e aumento da deambulação. O prognóstico é variável, dependendo do tipo de OI.
Última atualização: Jun 23, 2025
Osteogenesis imperfecta (OI) é uma doença hereditária do tecido conjuntivo caracterizada por défices na formação óssea e fragilidade óssea grave.
| Type I | Type II | Type III | Type IV | |
|---|---|---|---|---|
| Mutated gene | COL1A1, COL1A2 (collagen type 1 alpha 1 and 2 chains) | COL1A1, COL1A2, and CRTAP (cartilage-associated protein) | COL1A1, COL1A2 | COL1A1, COL1A2 |
| Inheritance modality | Autosomal dominant | Autosomal dominant AND autosomal recessive | Autosomal dominant | Autosomal dominant |
| Defect | Frameshift mutations in collagen type 1 alpha 1 and 2 chains leading to decreased amounts of normal collagen | Disrupted formation of the collagen triple helix structure, leading to little or no normal collagen | Mutations causing structural protein defects leading to severe pathology | Mutations causing structural protein defects leading to minimal or mild pathology |
| Type I | Type II | Type III | Type IV | |
|---|---|---|---|---|
| Description | Non-deforming with blue sclerae | Perinatally lethal | Progressively deforming | Variable with normal sclerae |
| Severity | Mild | Perinatal lethal | Severe | Mild to moderate |
| Fractures | < 100 | > 100 | > 100 | > 100 |
| Bone deformity | Uncommon | Severe | Moderate to severe | Mild to moderate |
| Stature | Normal to mildly reduced | Severely reduced | Reduced | Variable |
| Dentogenesis imperfecta | Variable | Common | Common | Variable |
| Color of sclerae | Blue | Dark blue | Blue | Normal to gray |
| Hearing loss | Present in approximately 50% | — | Frequent | Variable |

Blue-colored sclera associated with OI
Image: “Blue sclera” by the Department of Medical Oncology, Ankara University School of Medicine, 06300 Ankara, Turkey. License: CC BY 3.0.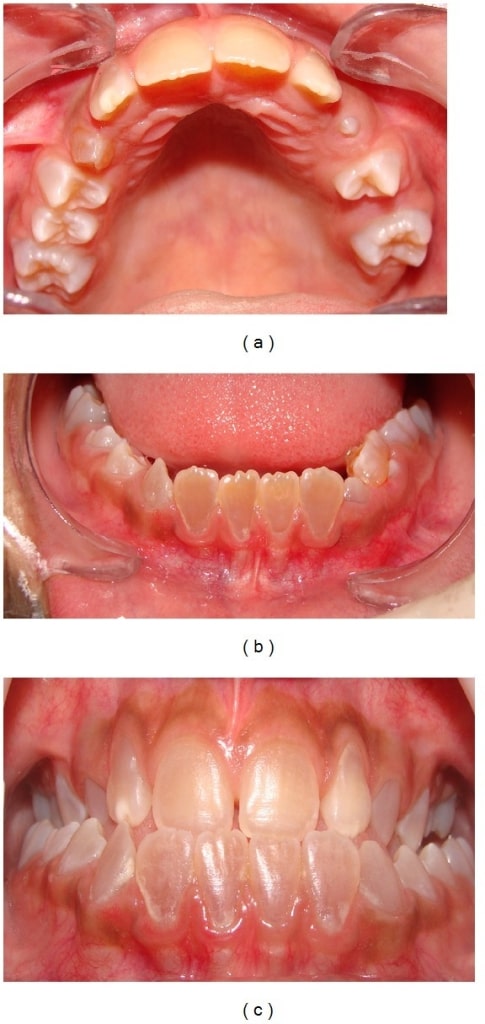
Dentinogenesis imperfecta:
Anterior teeth show a brownish discoloration (upper dental arch (a), lower arch (b), and dental occlusion(c)).

Intraoral photograph showing yellowish discoloration and chipping of the dentition: A 4-year-old male child with OI (type IV)
Image: “Chipping of the dentition” by the Department of Oral Medicine and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Mangalore 575018, India. License: CC BY 3.0.
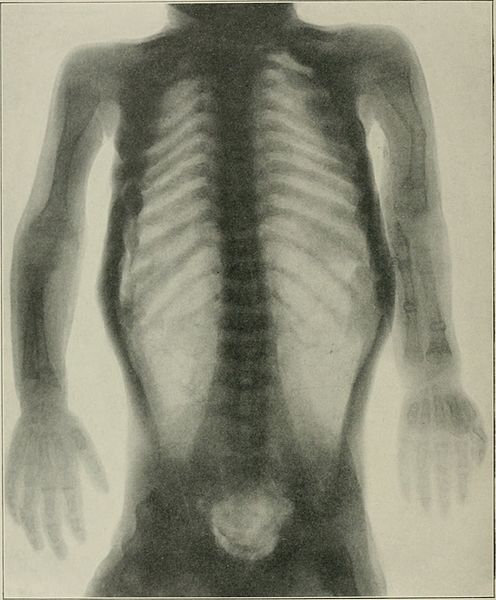
Infant with OI: Notice the deformity of the limbs, an indication of possible fractures during inspection.
Image: “Congenita A type of osteogenesis imperfecta” by the Maria Sklodowska Curie Clinical Emergency Hospital for Children, Bucharest, Romania. License: CC BY 2.0.| Type I | Type II | Type III | Type IV | |
|---|---|---|---|---|
| Skull radiographic findings | Intra-sutural bones | Undermineralization; calcified areas | Intra-sutural bones | Intra-sutural bones (sometimes) |
| Spine radiographic findings | Biconcave vertebrae (adults) | Widened vertebral bodies (platyspondyly) | Biconcave vertebrae; kyphoscoliosis | Biconcave vertebrae |
| Extremity radiographic findings | Thin cortices | Severely deformed femurs | Flared metaphyses, bowing, thin cortices | Thin cortices |
| Other radiographic findings | Osteopenia | Small, beaded ribs (pathognomonic) | Thin ribs, severe osteoporosis | Protrusio acetabuli in a subset |

Prenatal ultrasound diagnosing OI:
This prenatal ultrasound at 22 weeks’ gestation shows bowing of the femur (the crosshairs show the extremities of the femur).
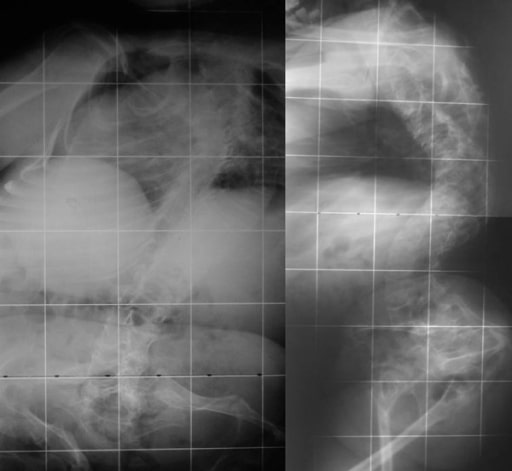
Radiograph showing OI:
periosteal dysplasia, almost complete absence of cortical bone, and numerous fractures

Chest radiograph showing long and narrow thorax (barrel-shaped chest) with anterior compression
Image: “Barrel-shaped chest” by the Department of Oral Medicine and Radiology, AB Shetty Memorial Institute of Dental Sciences, Nitte University, Mangalore 575018, India. License: CC BY 3.0.
Radiograph of the lower limbs showing bowing of the femur, with widening of the metaphases:
a 4-year-old boy with OI (type IV)

Radiograph showing a bowing tibia and fibula (saber shins):
a 4-year-old boy with OI (type IV)
Biconcave deformities in the lower thoracic and lumbar vertebrae in a 15-year-old patient with OI (“codfish” vertebrae)
Image: “Osteogenesis imperfecta” by the 1st Department of Orthopaedic Surgery, School of Medicine, University of Athens, “Attikon” Hospital, Rimini 1 Haidari 12462, Athens, Greece. License: CC BY 2.0.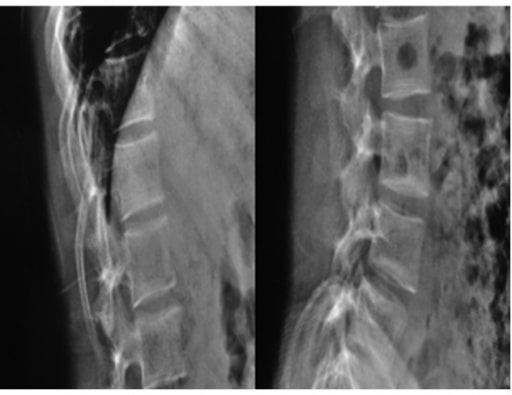
Radiographs of a 19-year-old woman with OI: Fragile bones, short trunk, severe kyphoscoliosis, and platyspondyly are noticed.
Image: “Biconcavity deformities” by the Department of Endocrine and Metabolic Diseases, Qilu Hospital, Shandong University, Jinan, Shandong 250012, P.R. China. License: CC BY 3.0.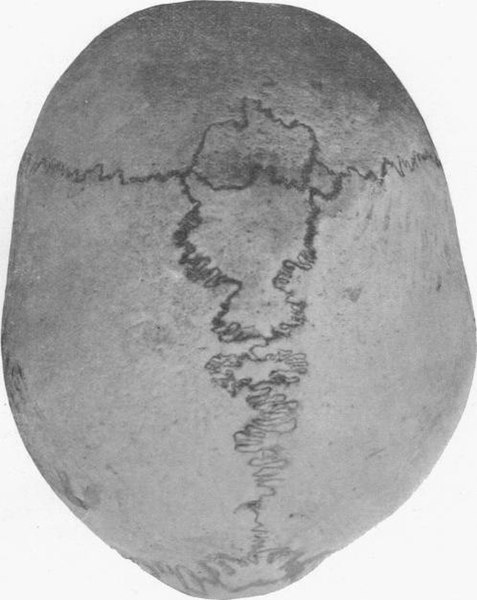
Human skull with wormian bones in a 21-year-old man
Image: “Wormian bones” by E. Barclay-Smith. License: Public domain.Não há cura definitiva para a OI.