A 2-year-old boy presents with multiple skin abscesses positive for Staphylococcus aureus. Past medical history is significant for recurrent infections by the same organism. The nitroblue tetrazolium (NBT) test demonstrates an inability to kill the microbes. Which of the following defects is most likely responsible for the findings in this patient?
A. Deficiency of CD40L on activated T cells
B. Tyrosine kinase deficiency blocking B cell maturation
C. Inability to generate the microbicidal respiratory burst
D. Inability to fuse lysosomes with phagosomes
E. MHC class II deficiency
A 55-year-old female presents with pain in both hands and wrists for the past several years. It is associated with morning stiffness that lasts for almost an hour. Physical examination reveals tenderness and swelling in both hands and wrists, most severe over the proximal interphalangeal joints. Laboratory investigation reveals the presence of anti-cyclic citrullinated peptide (anti-CCP). Which of the following immune-mediated injuries is responsible for this patient’s condition?
A. Self-tolerance
B. Both type II and III hypersensitivities
C. IgE-mediated immune responses only
D. Type IV hypersensitivity
E. Type III hypersensitivity
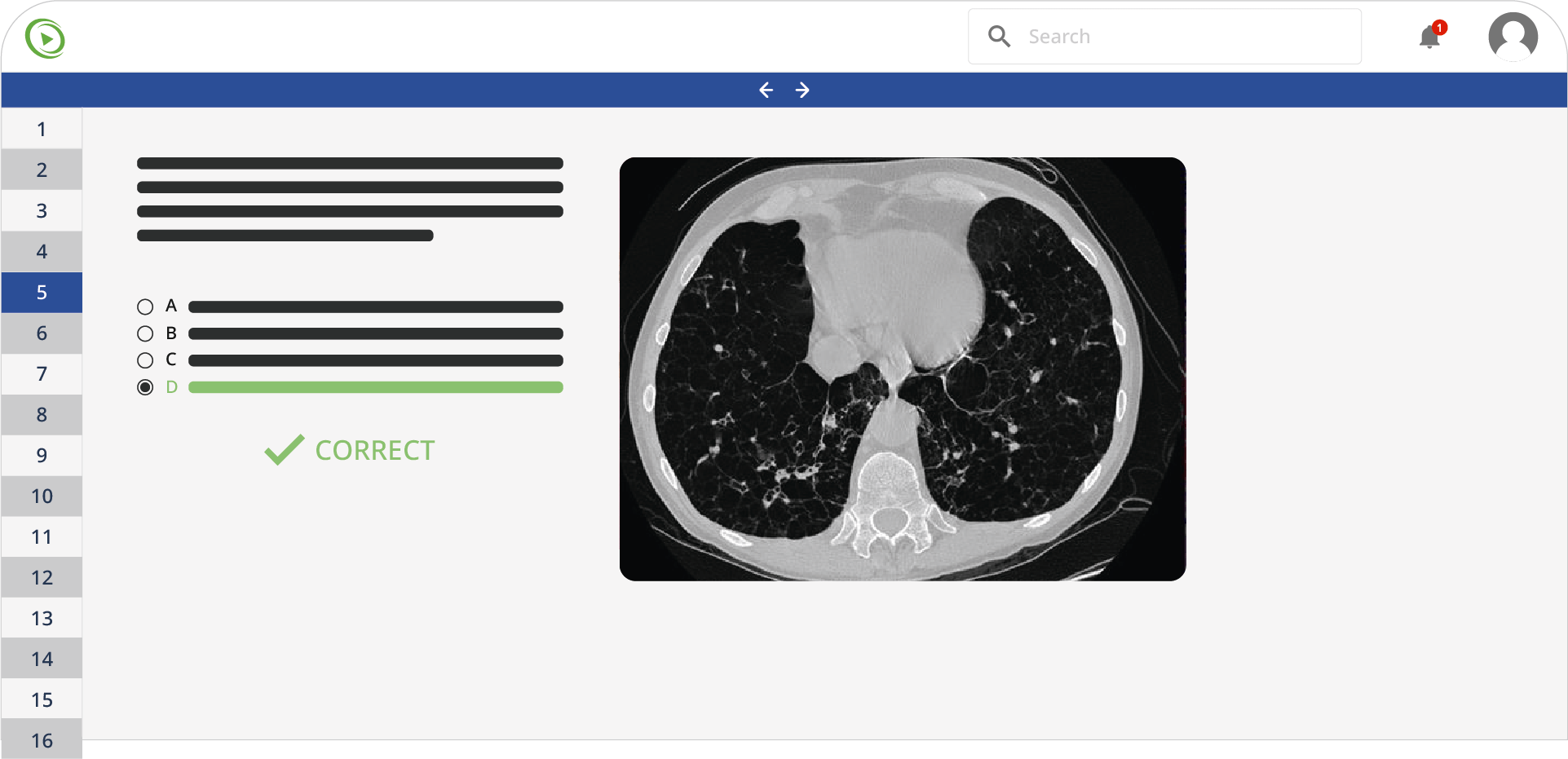
A 45-year-old man is transferred to the intensive care unit from the emergency department for acute respiratory failure. His medical history is significant for severe persistent asthma, hypertension, and several bouts of community and hospital-acquired pneumonia. His medications include amlodipine, lisinopril, inhaled fluticasone, salmeterol, and oral prednisone. He is a lifelong non-smoker and drinks alcohol occasionally on weekends. He works as a sales executive and visited Hawaii a month ago. In the emergency department, he was started on broad-spectrum antibiotics and bronchodilators. His respiratory failure progressively worsens, and on day 2 of admission, he requires mechanical ventilator support. Chest X-ray shows multiple nodules bilaterally in the lower lobes. Flexible bronchoscopy is performed and the bronchoalveolar lavage sample from the medial segment of the right lower lobe shows neutrophils, with the fungal preparation showing Aspergillus fumigatus. Video-assisted thoracoscopy is performed, and a biopsy from the right lower lobe is taken, which shows plugging of the terminal bronchioles with mucus, inflammatory cells, and fungal vascular invasion. Which of the following is the most likely mechanism responsible for the biopsy findings?
A. Impaired immune response due to medication
B. Production of a superantigen by A. fumigatus
C. Suppression of the production of IgA by A. fumigatus
D. Suppression of the production of IgM by A. fumigatus
E. Suppression of the innate immune system by A. fumigatus
A researcher is studying the mammalian immune response with an unknown virus. A group of mice are inoculated with the virus, and blood is subsequently drawn from these animals at various intervals to check immunoglobulin levels. Which of the following is a critical step in the endogenous pathway of antigen presentation for the virus model presented above?
A. Degradation of the antigen by the proteases in the phagolysosome
B. Translocation of the antigen into the endosome after phagocytosis
C. Translocation of the antigen into the endoplasmic reticulum via TAP proteins
D. Binding of the peptide to MHC class II
E. Interaction of the MHC class II complex with its target CD4+ T cell
A 21-year-old woman presents to her physician for a regular follow-up visit. She was diagnosed with relapsing-remitting multiple sclerosis 2 months ago when she suffered the 2nd episode of optic neuritis. She was successfully treated with methylprednisolone pulse therapy and discharged. Today, she only complains of slight fatigue with upper and lower extremity weakness. Her blood pressure is 120/80 mm Hg, the heart rate is 63/min, the respiratory rate is 14/min, and the temperature is 36.7°C (98.0°F). Neurological examination reveals brisk deep reflexes (3+ equal) and decreased strength (4/4) in the upper limbs. The rest of the examination is unremarkable. The patient is prescribed a drug that is an inhibitor of ɑ4-integrin (CD49d) for the prevention of relapses. She is concerned about the side effects of this drug, among which is increased susceptibility to the upper respiratory tract and urinary tract infections. Inhibition of which of the following processes is the best explanation for such adverse effects?
A. Tight adhesion of leukocytes to the endothelial cells
B. Expression of selectins on the surface of endothelial cells
C. Formation of tight bounds between leukocytes and endothelial selectins
D. Chemotaxis of leukocytes
E. Inhibition of the interaction between platelet endothelial cell adhesion molecules (PECAMs) on the surfaces of leukocytes and endothelial cells
A 16-year-old girl presents to her physician with itching, soreness, and irritation in the vulvar region. She reports that these episodes have occurred 6–7 times a year since the age of 5. She used to treat these symptoms with topical ketoconazole cream, but this time it failed to help. She also has had several episodes of oral candidiasis in the past. She is not sexually active and does not take any medication. Her vital signs are as follows: the blood pressure is 115/80 mm Hg, the heart rate is 78/min, the respiratory rate is 15/min, and the temperature is 35.5°C (97.7°F). Examination shows vulvovaginal erythema with cottage cheese-like plaques. Wet mount microscopy is positive for yeast. Along with a swab culture, the physician orders a dihydrorhodamine test and myelin peroxidase staining for a suspected primary immunodeficiency. The dihydrorhodamine test is positive, and the myeloperoxidase staining reveals diminished staining. Which of the following best describes this patient’s condition?
A. Her phagocytes are unable to generate an oxidative burst to kill intracellular bacteria
B. She is likely to have another immune impairment in addition to the 1 for which she was tested
C. She should receive prophylactic courses of wide-spectrum antibiotics to prevent infections
D. Her phagocytes can only perform extracellular killing
E. She is susceptible to all mycotic infections
A 7-year-old African-American boy presents to his physician with fatigue, bone and abdominal pain, and mild jaundice. The pain is dull and remitting, and the patient complains it sometimes migrates from 1 extremity to another. His mother reports that his jaundice and pain have occurred periodically for the past 5 years. At the time of presentation, his vital signs are as follows: the blood pressure is 80/50 mm Hg, the heart rate is 87/min, the respiratory rate is 17/min, and the temperature is 36.5°C (97.7°F). On physical examination, the patient appears to be pale with mildly icteric sclera and mucous membranes. On auscultation, there is a soft systolic ejection murmur, and palpation reveals hepatosplenomegaly. His musculoskeletal examination shows no abnormalities. Laboratory investigations show the following results:
| Complete blood count | |
| Erythrocytes | 3.7 x 106/mm3 |
| Hgb | 11 g/dL |
| Total leukocyte countNeutrophilsLymphocytesEosinophilsMonocytesBasophils | 7,300/mm351%40%2%7%0 |
| Platelet count | 151,000/mm3 |
| Chemistry | |
| Total bilirubin | 3.1 mg/dL (53 µmol/L) |
| Direct bilirubin | 0.5 mg/dL (8.55 µmol/L) |
A peripheral blood smear shows numerous sickle-shaped red blood cells. Among other questions, the patient’s mother asks you how his condition would influence his vaccination schedule. Which of the following statements is true regarding vaccination in this patient?
A. The patient should not receive meningococcal, pneumococcal, or Haemophilus influenzae vaccines, because they are likely to cause complications or elicit disease in his case.
B. The patient should receive serogroup B meningococcal vaccination at the age of 10 years.
C. The patient should receive serogroup D meningococcal vaccination as soon as possible because he is at a higher risk of getting serogroup B meningococcal infection than other children.
D. The patient should receive the pneumococcal polysaccharide vaccine as soon as possible, because he is at higher risk of getting pneumococcal infection than other children.
E. The patient’s condition does not affect his chances to get any infection; thus, additional vaccinations are not advised.
A 3-year-old toddler was rushed to the emergency department after consuming peanut butter crackers at a daycare. The daycare staff report that the patient has a severe allergy to peanut butter, and he was offered the crackers by mistake. The patient is in acute distress. His blood pressure is 60/40 mm Hg, respiratory rate is 27/min, and heart rate is 110/min. Upon examination, there is audible inspiratory stridor and his chest is covered in a maculopapular rash. Intubation is attempted and fails due to extensive laryngeal edema. The decision for cricothyrotomy is made. Which of the following is the most likely mechanism of this pathology?
A. C5a production
B. Release of IL-4
C. Deposition of antigen-antibody complexes
D. IL-2 secretion
E. C3b interaction
A 26-month-old boy is presented to the outpatient clinic by his parents complaining of a productive cough for the last 5 days. His mother reports a history of recurrent chest infections during the past year. He also has a history of chronic bloody diarrhea and pronounced bleeding after his circumcision. The vital signs are as follows: blood pressure 100/60 mm Hg, pulse 100/min, temperature 38.0°C (100.4°F), and respiratory rate 27/min. On examination, there are purpuric eruptions over the extremities as well as eczematous patches on the flexural surfaces of his elbows and knees. Chest auscultation reveals crepitus over the base of the right lung. Chest radiography is suggestive of consolidation in the right lower lobe. Blood test results show anemia, thrombocytopenia with small platelets, and leukopenia. With a suspicion of a congenital immunodeficiency, flow cytometry is ordered which reveals a Wiskott-Aldrich syndrome protein (WASP) mutation. Which of the following would be the definitive treatment of this patient’s condition?
A. Early hematopoietic stem cell transplantation (HSCT)
B. Intravenous immunoglobulin (IVIG)
C. Rituximab
D. Chemotherapy
E. Corticosteroids
A 10-year-old boy presents to the emergency department with sudden shortness of breath. He was playing in the school garden and suddenly started to complain of abdominal pain. He then vomited a few times. An hour later in the hospital, he slowly developed a rash on his chest, arms, and legs. His breathing became faster with audible wheezing. On physical examination, his vital signs are as follows: the temperature is 37.0°C (98.6°F), the blood pressure is 100/60 mm Hg, the pulse is 130/min, and the respiratory rate is 25/min. A rash is on his right arm, as shown in the image. After being administered appropriate treatment, the boy improves significantly, and he is able to breathe comfortably. Which of the following is the best marker that could be measured in the serum of this boy to help establish a definitive diagnosis?
Do you want to practice more Immunology questions?
Create a free Lecturio account and you’ll have access to the Lecturio question bank, with more than 2,200 USMLE Step 1 practice questions.