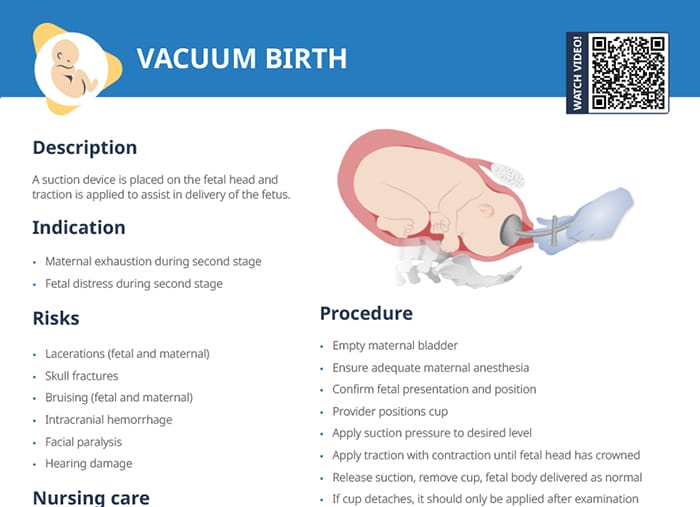
What is vacuum birth, or “vacuum-assisted delivery?”
In vacuum-assisted delivery, a suction device is placed over the vertex of the fetal head and traction is applied to assist in delivery of the fetus.
Related videos
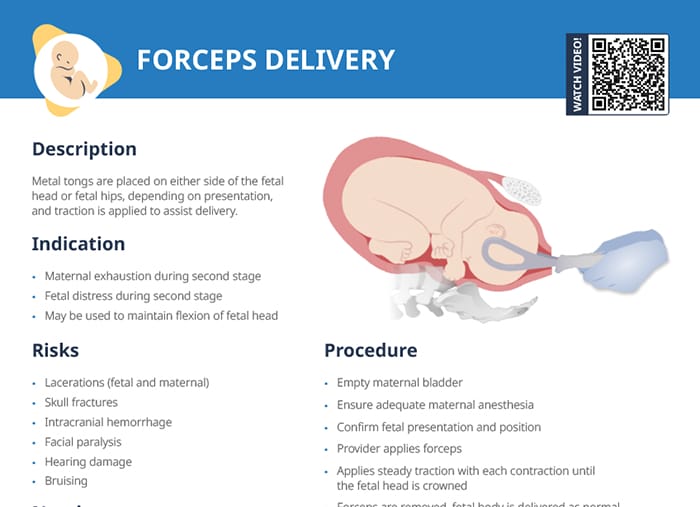
Indications and contraindications
Vacuum-assisted delivery is an option when the mother is exhausted in the second stage of labor. Adding the vacuum can help give more strength to the pushing power.
Fetal distress is another indication to speed up and assist the delivery process (shown by the Doppler/monitoring of fetal heart rate).
Vacuum birth is contraindicated in situations of:
- Incomplete cervical dilation
- Unengaged fetal head
- Non-vertex presentation
- Fetal prematurity (< 34 weeks)
- Suspected macrosomia
- Fetal scalp trauma
Risks and complications of vacuum-assisted birth
If the vacuum is poorly placed, the applied suction can lead to
- Fetal and maternal lacerations
- Skull fractures
- Bruising (fetal scalp and maternal vaginal walls)
- Intracranial hemorrhage
- Facial paralysis
- Hearing damage
Procedure
The procedure itself is performed by a provider. Nursing tasks include gathering equipment, monitoring the fetal heart rate, providing maternal support, and assessing the infant at delivery.
Tip: The most popular type of vacuum used is a “Kiwi.”
Clients should be informed on benefits and risks to mother and fetus prior to procedure and give clear consent (informed consent).
Clients should be aware that if vacuum assisted delivery is not successful, a cesarean section may be necessary.
Procedure steps:
- Empty maternal bladder
- Ensure adequate maternal anesthesia
- Confirm fetal presentation and position
- Provider positions cup
- Apply suction pressure to desired level
- Apply traction with contraction until fetal head has crowned
- Release suction, remove cup, fetal body delivered as normal
- If cup detaches, it should only be applied after examination of the fetal scalp (follow unit policy on number of times cup can be reapplied)