Nursing Knowledge
A T-tube is a transhepatic biliary catheter. It is a tube placed in the common bile duct that drains bile into a bag outside the body, allowing the bile duct time to heal.
T-tubes are most commonly placed after open cholecystectomies (removal of the gallbladder) and may remain in place for 2–6 weeks.
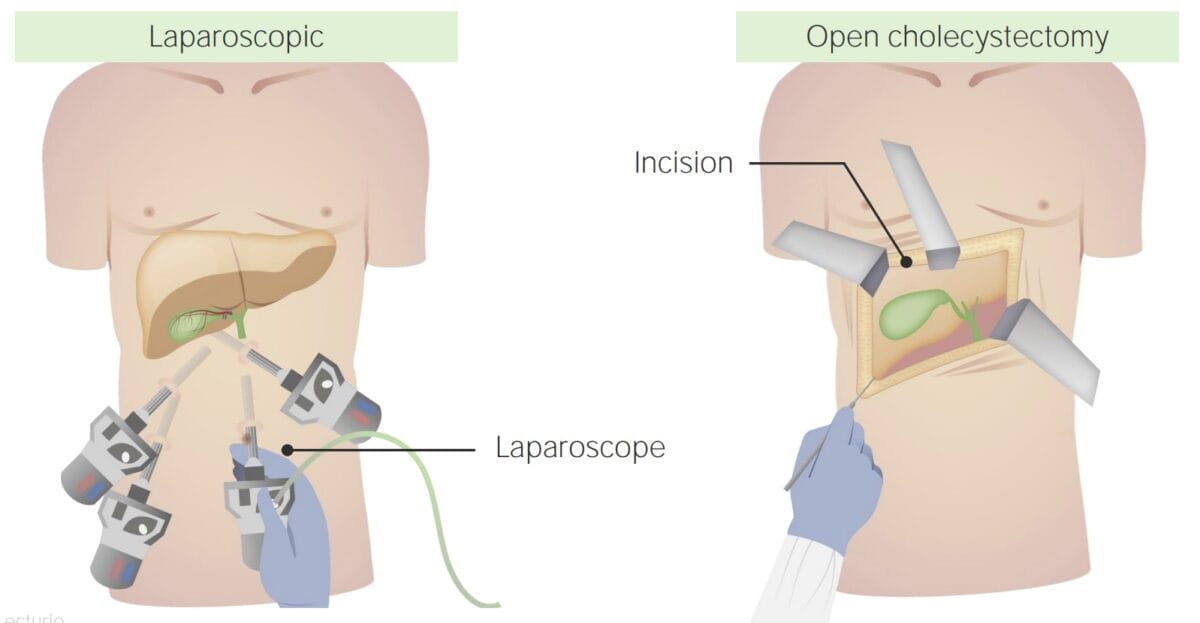
A cholecystectomy is a surgical procedure in which the gallbladder is removed. In an open or incisional cholecystectomy, it is removed through an incision in the abdominal wall. A T-tube may be placed in the common bile duct to keep the duct open while possible edema from manipulation during surgery resolves.
While placing a T-tube used to be a routine component of cholecystectomies, it is now only used in complicated cases, such as when a gallstone is retained in the common bile duct. Due to the increasingly common laparoscopic cholecystectomy and improved surgical techniques, T-tubes are needed less frequently.
Normally, the tube may drain up to 500 mL in the first 24 hours after surgery.
Drainage should decrease to less than 200 mL in 2–3 days and be minimal thereafter; with blood-tinged coloring initially changing to green-brown later on.
Priorities: Watch for signs of bleeding, bile leakage, T-tube obstruction, and infection. Monitor the client’s vital signs for signs of complications post-procedure, including fever and tachycardia.
Drainage:
Tube site:
Client comfort and education:
Clients should be encouraged to replace the amount of fluid drained into the T-tube bag with an electrolyte-rich liquid source.
Clients must be able to care for the T-tube following hospital discharge.
Instruct clients (how) to:
Further general education points:
Note: For many patients, the T-tube is not connected to a drainage bag when they leave the hospital. They need to flush it 1–2 times a day with 10 mL of sterile saline, and should be instructed to clean the cap and the end of the tube with alcohol before flushing.
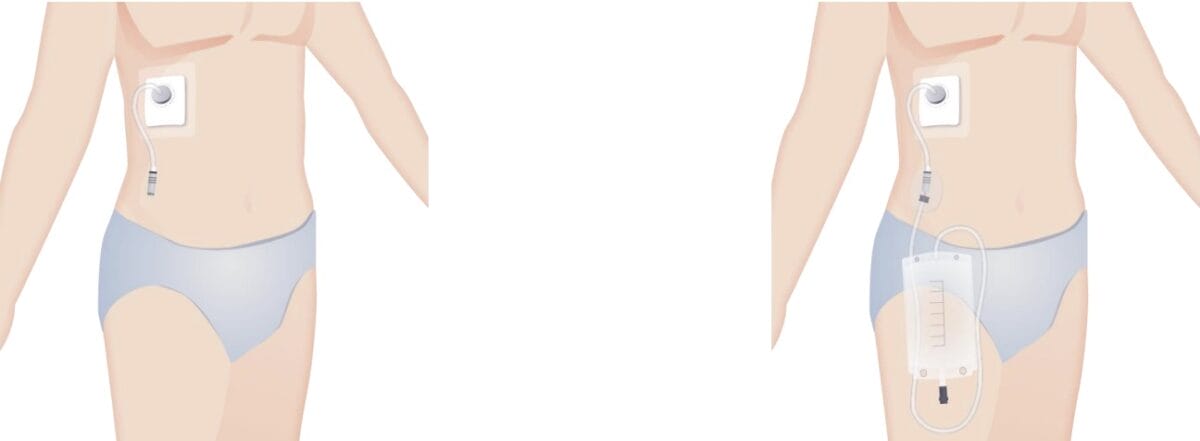
If a patient is sent home with a bag connected to the T-tube, further instructions are needed about how to empty the drainage bag:
Note: Clients often have a hard time keeping long lists like this in mind. You can summarize the points to watch for into categories such as “Signs the tube is blocked and not working” and “Signs of infection” to make it easier for the client to keep an overview.
The health care provider typically reviews an X-ray to ensure the duct has healed and there are no more stones before removing a T-tube.
RELATED TOPIC:
Free Download
Master the topic with a unique study combination of a concise summary paired with video lectures.
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Your free account gives you access to:
or
Have a holly, jolly study session 🎁 Save 50% on all plans now >>