What is systemic vascular resistance?
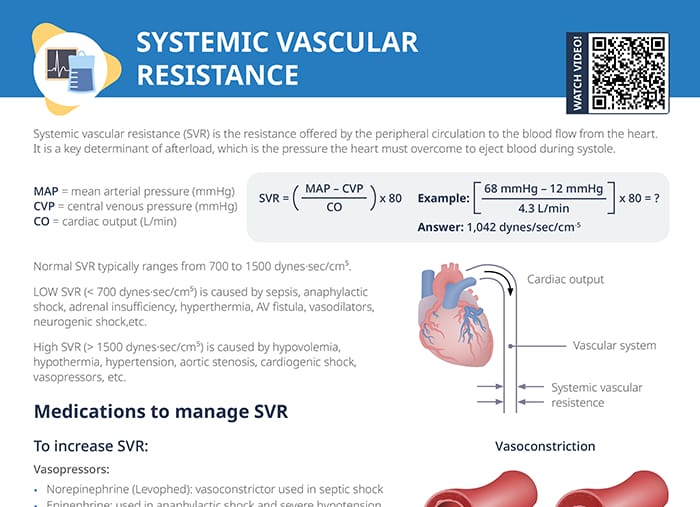
Systemic vascular resistance (SVR) is the resistance offered by the peripheral circulation to the blood flow from the heart.
SVR is a key determinant of afterload (= the pressure the heart must overcome to eject blood during systole).
Normal systemic vascular resistance (range)
Normal SVR typically ranges from 700 to 1500 dynes x sec/cm5.
Low SVR (< 700 dynes x sec/cm5) is caused by sepsis, anaphylactic shock, adrenal insufficiency, hyperthermia, AV fistula, vasodilators, neurogenic shock, etc. Low SVR can lead to inadequate perfusion of vital organs, so increasing the systemic vascular resistance to restore adequate blood pressure and perfusion is important for stabilization.
High SVR (> 1500 dynes x sec/cm5) is caused by hypovolemia, hypothermia, hypertension, aortic stenosis, cardiogenic shock, vasopressors, etc. Systemic vascular resistance that is too high can strain the heart and increases the risk for stroke, heart attacks, and kidney damage. Reducing the SVR is important to reduce the workload on the heart.
Formula to calculate systemic vascular resistance
The systemic vascular resistance is calculated using the mean arterial pressure, the central venous pressure, and the cardiac output.
$$ SVR = (\frac{MAP – CVP}{CO}) \times 80 $$MAP = mean arterial pressure (mmHg)
CVP = central venous pressure (mmHg)
CO = cardiac output (L/min)
Example
If the mean arterial pressure is 80 mmHg, the central venous pressure is 12 mmHg, and the cardiac output is 4.3 L/min, what is the systemic arterial pressure?
$$ [\frac{68 mmHg – 12 mmHg}{4.3 L/min}] \times 80 = ? $$Answer: 1042 dynes/sec/cm-5
Medications to increase low systemic vascular resistance
Vasopressors are used to increase SVR that is too low:
- Norepinephrine (Levophed): vasoconstrictor used in septic shock
- Epinephrine: used in anaphylactic shock and severe hypotension
- Dopamine: dose-dependent effects; higher doses increase SVR
Vasopressors constrict blood vessels, which raises blood pressure and systemic vascular resistance.
Nursing implications:
- Monitor blood pressure and signs of improved perfusion.
- Adjust dosage based on blood pressure targets and patient response.
- Watch for side effects like arrhythmias and excessive vasoconstriction.
Medications to decrease high systemic vascular resistance
Vasodilators are used to decrease SVR that is too high:
- Nitroglycerin: used in hypertensive emergencies and heart failure
- Sodium nitroprusside: for severe hypertension and heart failure
- ACE inhibitors (e.g., lisinopril): long-term management of hypertension
- Calcium channel blockers (e.g., amlodipine): manage hypertension by dilating blood vessels
Vasodilators lower SVR by causing vasodilation, which is important to lower blood pressure and reducing the risk of cardiovascular complications in hypertensive states.
Nursing implications:
- Monitor blood pressure and signs of hypotension.
- Adjust dosage to achieve a balance between lowering resistance and maintaining adequate perfusion.
- Monitor for adverse effects like dizziness, headaches, and potential over-dilation.