What are pressure ulcers?
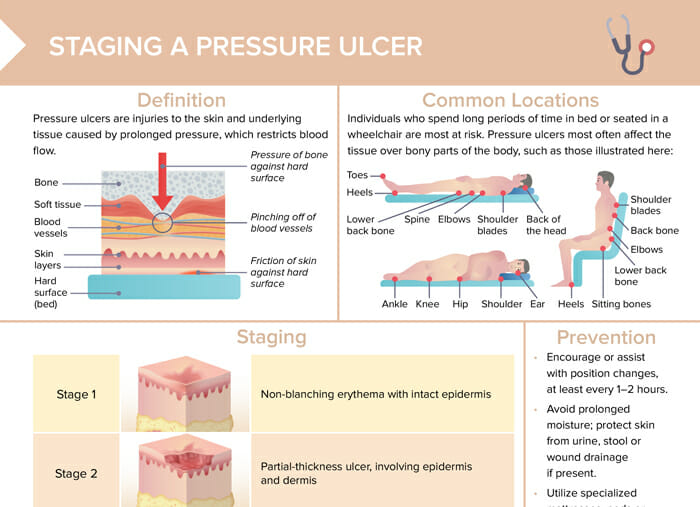
Pressure ulcers are injuries to the skin and underlying tissue caused by prolonged pressure restricting blood flow.
Nursing tip: Always do a full head-to-toe skin assessment upon admission or transfer to your unit, and document appropriately.
What causes pressure ulcers?
Pressure ulcers (older terms: bed sores, decubitus) are usually caused by prolonged pressure on the skin. Other causes include friction, shear, moisture, and contributing factors include poor nutrition, poor blood flow, lack of mobility, old age, or decreased sensation.
Individuals who spend long periods of time in bed or seated in a wheelchair are most at risk.
What are common locations of pressure ulcers?
Pressure ulcers most often affect the tissue over bony parts of the body.
When lying on the back:
- Toes
- Heels
- Lower back bone
- Spine
- Elbows
- Shoulder blades
- Back of the head
When lying on the side:
- Ankle
- Knee
- Hip
- Shoulder
- Ear
When sitting:
- Heels
- Sitting bones
- Lower back bone
- Elbows
- Back bone
- Shoulder blades
What are the 4 stages of pressure ulcers?
Table: Stages of pressure ulcers
| Stage 1 | Non-blanching erythema with intact epidermis |
| Stage 2 | Partial-thickness ulcer, involving epidermis and dermis |
| Stage 3 | Full-thickness ulcer extending through dermis into subcutaneous tissue |
| Stage 4 | Deep tissue destruction extending through fascia; may involve muscle, bone, tendon |
| Unstageable | Depth of injury unknown due to presence of necrotic tissue or eschar; surgical debridement required for staging |
How to prevent pressure ulcers
Measures that can be taken to help prevent pressure ulcers include:
- Encourage or assist with position changes, at least every 1–2 hours.
- Avoid prolonged moisture; protect skin from urine, stool or wound drainage.
- Utilize specialized mattresses, pads or cushions to relieve and redistribute pressure.
- Maintain tissue integrity with a well-balanced, protein-rich diet
How are pressure ulcers treated?
Treatment depends on the stage and severity. General approaches include:
- Relieving pressure on the affected area
- Cleaning and dressing wounds using appropriate dressings
- Debridement (removal of dead tissue)
- Providing proper nutrition to support healing
- Administering antibiotics if there’s an infection