What are restraints in nursing?
In nursing, restraints are used as a last resort to ensure patient and staff safety. They are categorized into behavioral and non-behavioral types:
- Behavioral restraints: These are used to manage violent or self-destructive behavior that poses an immediate danger to the patient or others. Examples include wrist and ankle restraints, and sometimes seclusion rooms.
- Non-behavioral (medical) restraints: These are used to limit movement for medical safety, such as preventing a patient from removing IV lines or interfering with life-support equipment. Examples include mittens, limb holders, or bed rails.
Both types require regular assessment, strict documentation, and the least restrictive option should always be considered first. Ethical and legal guidelines must be followed, including obtaining informed consent when possible.
Types of restraints in nursing
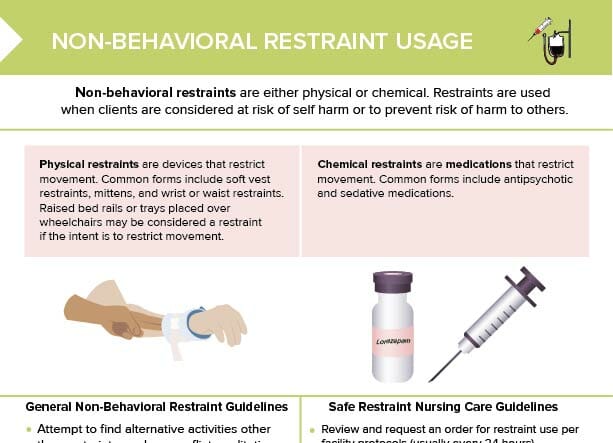
Restraints are either physical or chemical.
Physical restraints are devices that restrict movement. Common forms include soft vest restraints, mittens, and wrist or waist restraints. Raised bed rails or trays placed over wheelchairs may be considered a restraint if the intent is to restrict movement.
Chemical restraints are medications that restrict movement. Common forms include antipsychotic and sedative medications.
What are soft restraints?
Soft restraints are devices made of padded material.
What are wrist restraints?
Wrist restraints are bands or cuffs wrapped around a client’s wrists to limit hand and arm movement.
What are vest restraints?
Vest restraints are vests or jackets that are put on a client and attached to the bed. They allow for some mobility, but restrict upper-body movement and help prevent clients leaving the bed without assistance and falling.
How to tie restraints
Important tips to keep in mind when tying physical restraints (like wrist restraints):
- Use soft or padded material that will not injure skin
- Always use a quick-release knot so that restraint can be removed swiftly in case of emergency
- Take care that the restraint is not tied too tight (2-finger rule)
- Attach the restraint to a part of the bed frame that moves with the patient to reduce risk of injury
- Carefully monitor the restrained client and document the procedure
General non-behavioral restraint guidelines
- Attempt to find alternative activities other than restraints, such as closer room assignments, offer diversional activities (puzzle, music), trained sitter,
- Assess for client needs such as hunger, thirst, or toileting.
- Review facility guidelines for restraints.
- Obtain a restraint use order from a provider.
- Conduct a baseline client assessment.
- Understand the difference between physical and chemical restraints.
- Educate client and caregivers on restraint use.
- Document per facility protocol.
Safe restraint nursing care guidelines
- Review and request an order for restraint use per facility protocols (usually every 24 hours).
- Monitor and assess client at least every 2 hours and offer food, water, position changes, and toileting.
- Perform range of motion exercise when appropriate.
- Conduct skin checks and skin care at least every 2 hours.