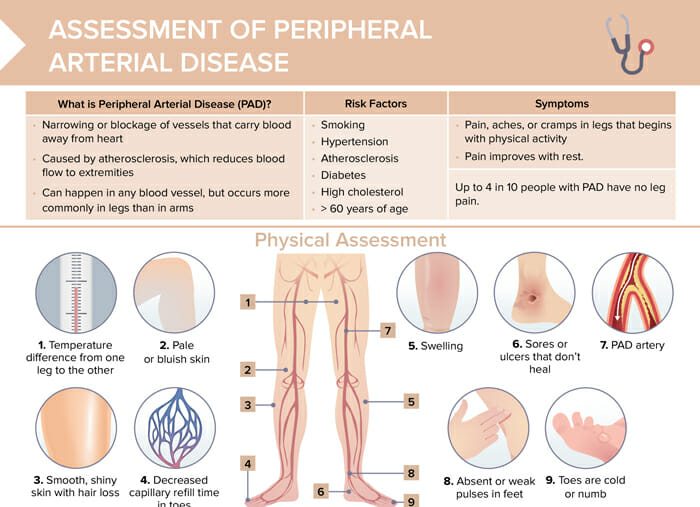
What is peripheral artery disease?
Peripheral artery disease (PAD) is a narrowing or blockage of vessels that carry blood away from the heart. It is caused by atherosclerosis, which reduces blood flow from the extremities. PAD can happen in any blood vessel, but occurs more commonly in the legs than in the arms.
Risk factors for PAD
- Smoking
- Hypertension
- Atherosclerosis
- Diabetes
- High cholesterol
- > 60 years of age
Peripheral artery disease: screening
Factors indicating a need for screening are risk factors that include: age over 65 or age over 50 with a history of diabetes or smoking; symptoms of leg pain; healing issues; absent pulses. Screening is typically done with the ankle-brachial index test.
How to diagnose PAD
The ankle-brachial index (ABI) test can be used to diagnose PAD.
The test compares blood pressure between the upper and lower extremities.
Highest systolic ankle pressure/highest brachial systolic pressure = ABI.
Classification of PAD according to ABI
| > 1.4 | Vessel hardening |
| 1.0–1.4 | Normal |
| 0.9–1.0 | Acceptable |
| 0.8–0.9 | Mild arterial disease |
| 0.5–0.8 | Moderate arterial disease |
| < 0.5 | Severe arterial disease |
Additional possible testing:
- Exercise ABI test
- Blood work (lipids, glucose)
- 6-minute walking test
- Doppler ultrasound
- Computed tomography angiography
- Magnetic resonance angiography
- Catheter-based angiography
How is peripheral artery disease treated?
Peripheral artery disease is treated through a multi-faceted approach:
- Angioplasty: A catheter with a balloon is inserted into the narrowed artery. The balloon is inflated to widen the artery, and sometimes a stent is placed to keep it open. Nurses prep patients, monitor them during the procedure, and provide post-procedure care like assessing for complications.
- Physical exercise: Supervised exercise programs improve walking distance and alleviate symptoms. Nurses often help patients tailor exercise programs and monitor progress.
- Heart-healthy diet: Low-fat, low-cholesterol, and high-fiber diets help manage PAD. Nurses educate patients on diet changes and may coordinate with dietitians.
Each modality aims to improve blood flow, alleviate symptoms, and prevent disease progression.
What is the best sleeping position for peripheral artery disease?
While individual comfort varies widely, elevating the legs is discouraged, as this position can decrease arterial blood flow to the legs, exacerbating symptoms.
What is peripheral venous disease?
Peripheral venous disease (PVD), often just called venous disease, refers to conditions that affect the veins of the peripheral system, typically in the legs. Unlike PAD which involves narrowed or blocked arteries, PVD is characterized by issues with veins, especially the valves inside them.
The most common form of PVD is chronic venous insufficiency (CVI). In CVI, the vein valves that prevent blood from flowing backward become damaged or weak, leading to blood pooling in the legs.
Risk factors for venous disease
- Older age
- Gender (women at higher risk)
- Smoking
- Obesity
- Sedentary lifestyle
- Pregnancy
- History of family being affected, or previous DVT
How to diagnose PVD
Diagnosis of PVD includes combining clinical factors with tests:
- History and examination (pain, heaviness, swelling, varicose veins)
- Duplex ultrasound (identify valve dysfunction)
- Venography (visualize vein conditions)
- D-dimer test (identify/rule out blood clots)
- ABI (rule out PAD)
How is peripheral venous disease treated?
Effective management of PVD often requires compression therapy (often first-line treatment), medications (diuretics, anticoagulants), lifestyle modifications (exercise, leg elevation), and, in some cases, surgical interventions (vein stripping, laser surgery).
How to recognize and differentiate PAD and PVD (symptoms)
The most significant peripheral artery disease symptom is pain, aches, or cramps that begin with physical activity. The pain improves with rest. It is to note that up to 4 in 10 people with PAD have no leg pain. Other specific symptoms of PAD include
- Temperature difference from one leg to the other
- Pale or bluish skin
- Smooth, shiny skin with hair loss
- Decreased capillary refill time in toes
- Swelling
- Sores or ulcers that don’t heal
- PAD artery
- Absent or weak pulses in feet
- Cold or numb toes
In peripheral venous disease, affected clients also suffer from leg pain, but this is not usually relieved by rest. The leg pain is persistent and characterized by “heaviness.” Swelling in legs and ankles is exacerbated by prolonged standing. Strong, palpable pulses are present, but may be hard to find due to edema. Further symptoms of PVD:
- Itching, tingling
- Hyperpigmentation/eczema/ulceration around the ankles
- Varicose veins
Nursing interventions for PAD and PVD
Patient education and administering prescribed medications are important nursing interventions for both conditions.
Important nursing interventions for PAD
- Pain management
- Skin care for ulcers or sores
- Assessing and monitoring for signs of decreased perfusion
Important nursing interventions for PVD
- Compression therapy
- Leg elevation