Video: How the body changes after pregnancy
Related videos
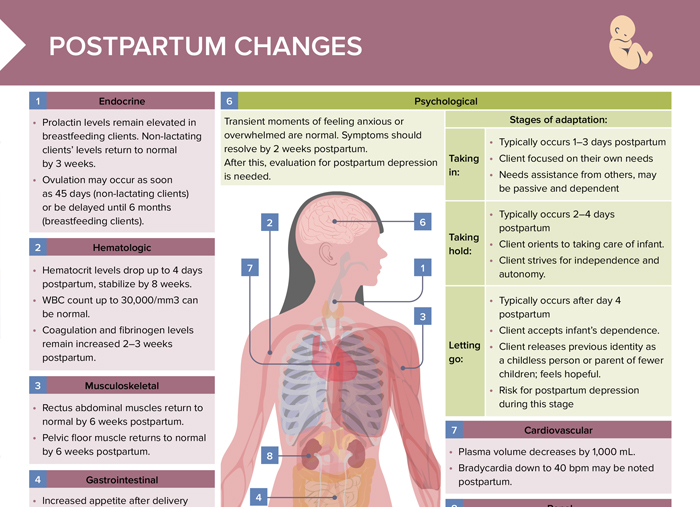
Endocrine postpartum changes
- Prolactin levels remain elevated in breastfeeding clients. Non-lactating clients’ levels return to normal by 3 weeks.
- Ovulation may occur as soon as 45 days (non-lactating clients) or be delayed until 6 months (breastfeeding clients).
Hematologic postpartum changes
- Hematocrit levels drop up to 4 days postpartum, stabilizes by 8 weeks.
- WBC count up to 30,000/mm3 can be normal.
- Coagulation and fibrinogen levels remain increased 2–3 weeks postpartum.
Musculoskeletal postpartum changes
- Rectus abdominal muscles return to normal by 6 weeks postpartum.
- Pelvic floor muscle returns to normal by 6 weeks postpartum.
Gastrointestinal postpartum changes
- Increased appetite after delivery
- Bowel movement may be delayed 2–3 days.
- Breastfeeding clients need an additional 300–500 calories per day to support lactation.
Reproductive postpartum changes
- Breasts: colostrum present first 3 days, then changes to mature milk stimulated by breastfeeding
- Non-breastfeeding clients should avoid any breast stimulation. Milk production may take several days, up to several weeks, to stop.
- While breast engorgement can be normal postpartum, signs of mastitis require further evaluation and treatment.
- Uterus involutes 1 cm/day (non-palpable by 2 weeks postpartum).
- Cramping may be stronger in multiparous and breastfeeding clients.
- Cervix: os appears slit-like instead of circular, returns to 1 cm dilation by 1 week postpartum.
- Lochia is normal discharge that contains blood, mucus, and uterine tissue and may last up to 6 weeks postpartum.
- Lochia rubra: bright red, days 1–3
- Lochia serosa: pink, days 4–10
- Lochia alba: white/yellow, days 11–6 weeks
Psychological postpartum changes
Transient moments of feeling anxious or overwhelmed are normal. Symptoms should resolve by 2 weeks postpartum. After this, evaluation for postpartum depression is needed.
Stages of adaptation:
- Taking in:
- Typically occurs 1–3 days postpartum
- Client focused on their own needs
- Needs assistance from others, may be passive and dependent
- Taking hold:
- Typically occurs 2–4 days postpartum
- Client orients to taking care of infant
- Client strives for independence and autonomy
- Letting go:
- Typically occurs after day 4 postpartum
- Client accepts infant’s dependence
- Client releases previous identity as a childless person or parent of fewer children; feels hopeful
- Risk for postpartum depression during this stage
Cardiovascular postpartum changes
- Plasma volume decreases by 1,000 mL.
- Bradycardia down to 40 bpm may be noted postpartum.
Renal postpartum changes
- Diuresis occurs after first 12 hours postpartum, up to 3,000 mL/day.
- Dilated ureters and renal pelvis returns to normal by 6–8 weeks postpartum.
Postpartum nursing diagnosis
Potential postpartum nursing diagnoses include:
- Acute pain related to perineal trauma, episiotomy, C-section, post-birth contractions
- Fatigue related to childbirth, body changes and new responsibilities
- Impaired urinary elimination related to trauma/swelling or anesthesia effects
- Risk for constipation related to hormonal changes, fear of pain with defecation, medications or anesthesia effects
- Postpartum depression
- Disturbed sleep pattern
- Impaired physical mobility
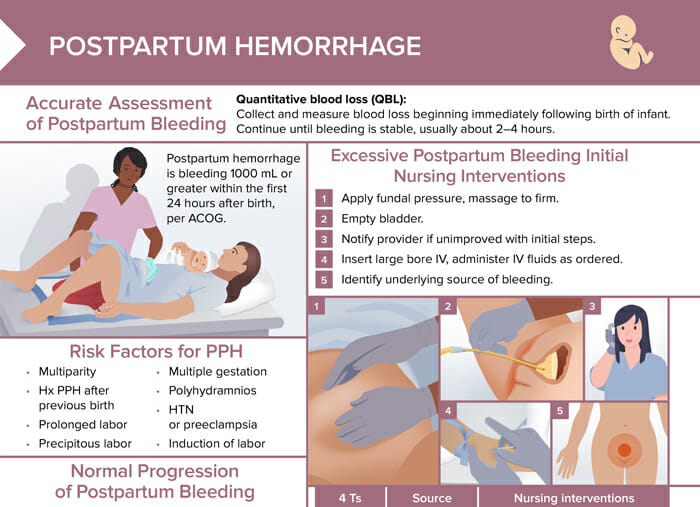
- Risk for hemorrhage
- Risk for infection
- Risk for impaired parent/infant attachment
- Risk for ineffective breastfeeding