What is a postpartum hemorrhage?
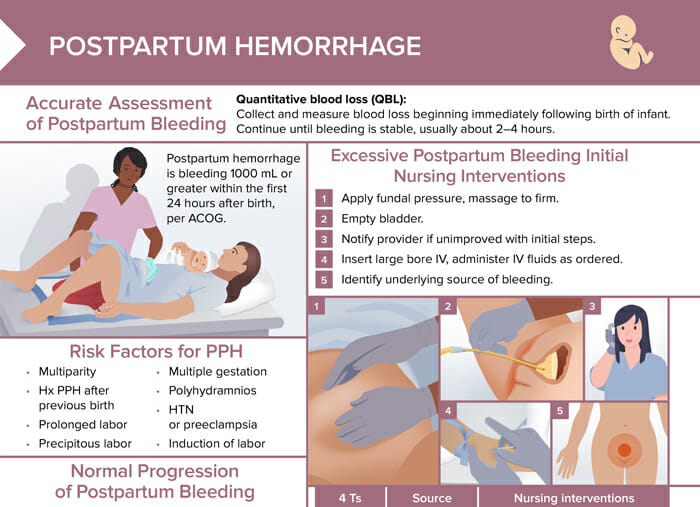
Postpartum hemorrhage (PPH) is defined as significant loss of blood following childbirth. It is one of the leading causes of maternal mortality worldwide.
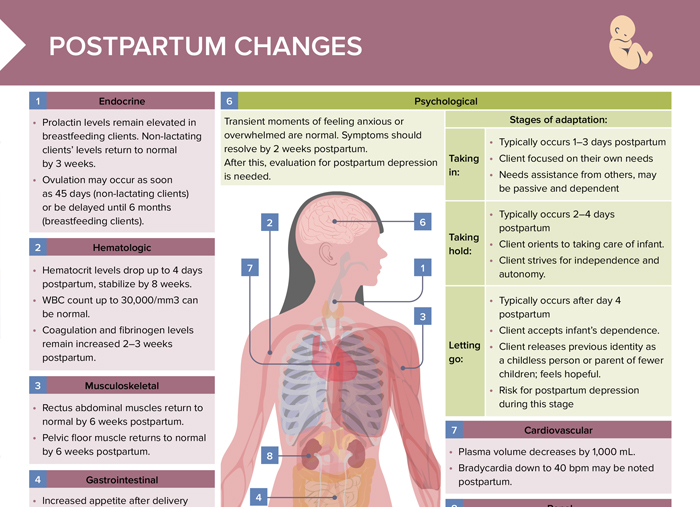
How much blood loss is considered postpartum hemorrhage?
Postpartum hemorrhage (PPH) is defined as loss of > 500 mL of blood after vaginal birth or > 1000 mL after cesarean section within 24 hours of delivery.
What are the different types of postpartum hemorrhage?
Postpartum hemorrhage (PPH) can occur at two primary times:
- Primary (or immediate) PPH:
- Most common
- Occurs within the first 24 hours after childbirth
- Usually due to the uterus failing to contract properly after birth (uterine atony), trauma to the birth canal, or complications from a retained placenta.
- Secondary (or delayed) PPH:
- Occurs between 24 hours and 12 weeks postpartum
- Caused by retained placental fragments, infection, or subinvolution of the uterus
Related videos
What causes postpartum hemorrhage?
The most common causes of PPH can be summarized as the “4 Ts:”
- Tone:
- Most common cause of PPH
- Uterus fails to contract after birth (uterine atony) → blood vessels are not compressed and continue to bleed
- Trauma: lacerations in the birth canal (tears, cuts); uterine rupture/inversion
- Tissue: placental fragments or other tissues remain in the uterus, which can prevent the uterus from contracting properly, leading to excessive bleeding
- Thrombin: coagulopathies
What are the risk factors for postpartum hemorrhage?
- Multiparity
- Hx PPH after previous birth
- Prolonged labor
- Precipitous labor
- Multiple gestation
- Polyhydramnios
- HTN or preeclampsia
- Induction of labor
It is important to note that postpartum hemorrhage can occur in clients without any risk factors. Clients should be educated about the signs and symptoms of PPH (heavy bleeding, large clots, light-headedness, rapid heartbeat) so they can seek immediate medical attention.
How to prevent postpartum hemorrhage
Actively managing the third stage of labor has the biggest impact in reducing the risk of postpartum hemorrhage. This includes the administration of uterotonic drugs immediately after birth and uterine massage after placenta delivery.
Other measures are:
- Identifying risk factors early on (like previous PPH, multiple pregnancies, etc) and taking precautions
- Treating anemia and paying attention to proper nutrition during pregnancy to make body more resilient to blood loss
- Ensuring all providers are well-trained in recognizing and treating PPH, as quick intervention is crucial when PPH does occur
How to stop postpartum bleeding fast: initial nursing interventions
- Apply fundal pressure, massage to firm.
- Empty bladder.
- Notify provider if unimproved with initial steps.
- Insert large bore IV, administer IV fluids as ordered.
- Identify underlying source of bleeding.
How is postpartum hemorrhage treated?
Further nursing interventions depend on the cause of the bleeding:
- For uterine atony, administer uterotonic medications as ordered and assist with placement of Bakri balloon as needed.
- For retained placental fragments, prepare client for removal (possibly in OR).
- For lacerations, uterine rupture or inversion, prepare client for inspection by provider. Assist with positioning/visualization during inspection and repair as needed.
- For coagulation disorders, draw lab work as needed.
How to monitor and assess for PPH
Quantitative blood loss (QBL): Collect and measure blood loss beginning immediately following birth of infant. Continue until bleeding is stable, usually about 2–4 hours.
What are the different types of normal postpartum bleeding?
The different types of postpartum bleeding are:
- Lochia rubra: bright/dark red, lasts for 3–4 days after birth
- Lochia serosa: pinkish/brown, lasts for 4–12 days
- Lochia alba: yellow/white, lasts from 12 days to 3 weeks