What is “baby blues” vs postpartum depression?
The “baby blues” is a term for normal emotional changes during the first two weeks postpartum. They affect 80% of birthing people and resolve spontaneously.
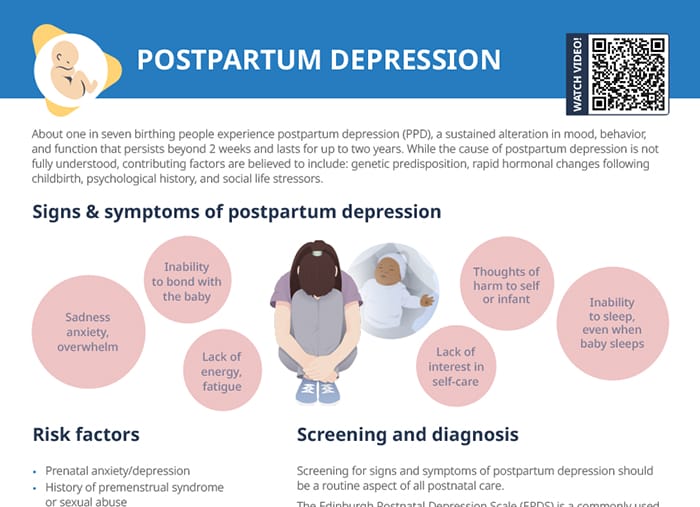
Postpartum depression is defined as a sustained alteration in mood, behavior, and function that persists beyond 2 weeks. It can last up to two years.
How common is postpartum depression?
Postpartum depression affects about one in seven people after giving birth.
What causes postpartum depression?
The cause of postpartum depression is not fully understood. Contributing factors are believed to include genetic predisposition, the rapid hormonal changes following childbirth, and other risk factors including:
- Prenatal anxiety/depression
- History of premenstrual syndrome or sexual abuse
- Traumatic labor/birth experience
- Recent stressful life events
- Inadequate social support
- Unhealthy or abusive primary relationship
Signs and symptoms of postpartum depression
Signs
- Sadness, anxiety, overwhelm
- Inability to bond with the baby
- Lack of energy, fatigue
- Lack of interest in self-care
- Thoughts of harm to self or infant
- Inability to sleep, even when baby sleeps
Screening and diagnosis
Screening for signs and symptoms of postpartum depression should be a routine aspect of all postnatal care.
The Edinburgh Postnatal Depression Scale (EPDS) is a commonly used screening tool. It is a 10-item self-report questionnaire, with each question evaluating the presence of typical symptoms. Each item is scored on a scale from 0 to 3, with a maximum score of 30. Higher scores indicate a greater likelihood of depression. Follow-up is necessary when:
- Score is greater than or equal to 13
- Any suicidal ideation is present
Treatment
Non-pharmacological approaches
- First-line treatment in mild to moderate PPD
- Talk therapy
- Cognitive behavioral therapy (CBT)
- Postpartum support groups
- Transcranial magnetic stimulation (TMS)
Pharmacological approaches
- Recommended in combination with psychotherapy in moderate to severe PPD
- SSRIs (first line)
- SNRIs
- Mirtazapine
Client family questions and nursing care
Identify clients with risk factors prenatally and provide proactive support and referral. Establish lines of communication for clients and family members to ask for support when needed. Know the resources available in your area and nationally and establish referral protocols that avoid delays in care.
“How do you know if you have postpartum depression?”
Educate clients about “baby blues” and make sure to explain the signs and symptoms of PPD from the normal mood fluctuations. The main indicator of PPD is that the symptoms persist after about two weeks postpartum.
“How to help my wife with postpartum depression”
Include partners and other support people in education. Outside of assisting with baby care, they can watch out for the signs of PPD, provide emotional support by being present and expressing reassurance, as well as be informed about the options for professional help and encourage it if needed.
“How long can you get disability for postpartum depression?”
The duration varies based on the individual case’s severity, the specific policies, and regional regulations. Refer clients to the relevant sources of information. Generally, many short-term disability insurance policies cover PPD for a period of 6 to 12 weeks. In some cases, long-term benefits or taking FMLA leave may be available options.