What is polypharmacy?
Polypharmacy refers to the use of multiple medications by a single individual. Sometimes, this can mean the client is using even more medications than clinically indicated.
Polypharmacy in older adults
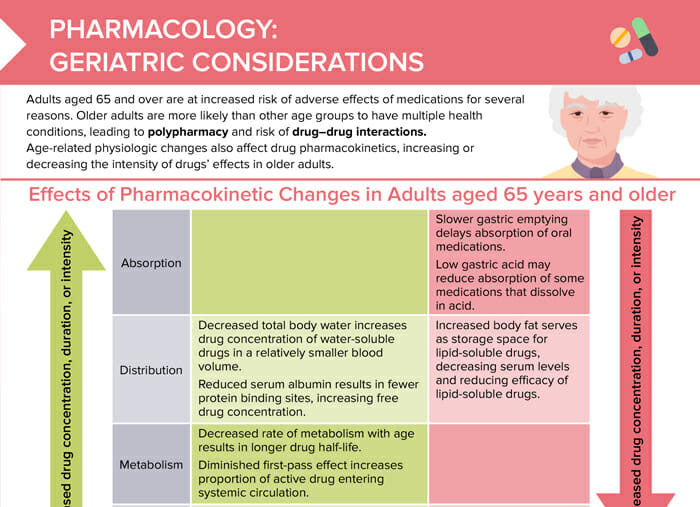
Polypharmacy becomes especially relevant in geriatric clients due to the multiple comorbidities from diagnoses. The need for multiple medications increases the risk of drug–drug interactions, which is why the complete list of medications taken by older clients needs to be closely monitored. Age-related physiologic changes also affect drug pharmacokinetics, increasing or decreasing the intensity of the many drugs’ effects in older adults, making the medication management in older adults more complex.
What age is geriatric for pharmacology?
Adults aged 65 and over are counted as geriatric and are at increased risk of adverse effects of medications.
Medication risks and considerations in geriatric patients
Factors leading to risk of overdosing
Factors that lead to increased drug concentration, duration, or intensity in older adults include:
- Decreased total body water in older adults increases drug concentration of water-soluble drugs in a relatively smaller blood volume.
- Reduced serum albumin results in fewer protein binding sites, increasing free drug concentration.
- Decreased rate of metabolism with age results in longer drug half-life.
- Diminished first-pass effect increases proportion of active drugs entering systemic circulation.
- Decreased renal blood flow and filtration rate allow greater accumulation of the drug in the bloodstream.
Factors leading to risk of underdosing
Factors that lead to reduced drug concentration, duration, or intensity in older adults include:
- Slower gastric emptying delays absorption of oral medications.
- Low gastric acid may reduce absorption of some medications that dissolve in acid.
- Increased body fat serves as storage space for lipid-soluble drugs, decreasing serum levels and reducing efficacy of lipid-soluble drugs.
Other factors affecting medication safety in older clients
- Higher risk of drug–drug interactions due to polypharmacy
- Increased sensitivity to side effects
- Drug–disease interactions (one drug for one condition may exacerbate another)
- Unintentional non-compliance due to cognitive decline
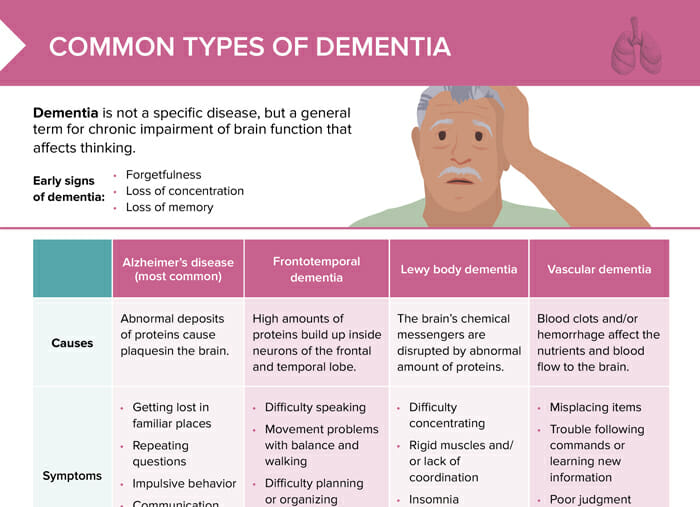
- Monitor cognitive issues like confusion, dementia, delirium due to some medications.
Nursing interventions for better medication safety in older adults
- Obtain a complete list of client medications, including over-the-counter medications, vitamins, and supplements.
- Utilize BEERS criteria to assess safety and appropriateness of client’s medication list.
- Collaborate with a pharmacist to identify potential drug–drug interactions.
- Assess for physical changes that may impact the client’s ability to follow medication plans and provide accommodations as needed.
- Adapt medication education if vision, hearing loss, or other age-related changes are present. Use return demonstration or teach–back to confirm understanding.
BEERS criteria
The BEERS criteria are a tool to assist health care providers in assessing
- Benefits
- Efficacy
- Evidence, and
- Risks
to improve medication safety for older adults. Using this template helps identify potentially inappropriate drugs, potential drug–drug interactions, and renal dosing adjustments.