What is placenta previa? Definition
Placenta previa occurs when the placenta implants in the lower uterine segment, rather than the fundus, and therefore covers the cervical os. If the placenta covers the cervix, it blocks the birth canal and presents the risk of life-threatening bleeding when the cervix begins to dilate.
Related videos
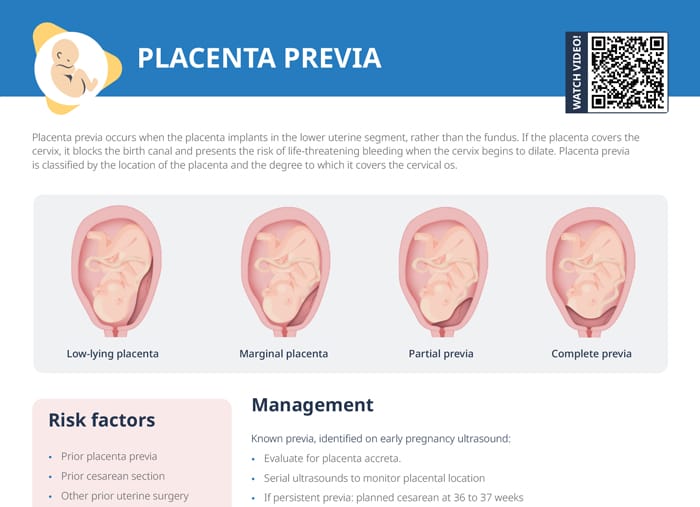
Placenta previa types
Placenta previa is classified by the location of the placenta and the degree to which it covers the cervical os.
Low-lying placenta
A low-lying placenta is located in the lower part of the uterus, but does not reach the cervix and does not cover it at all. Monitoring and expectant management may be considered here, since this type may resolve as the pregnancy progresses.
Marginal placenta previa
In marginal placenta previa, the placenta is at the edge of the cervix, not covering it fully, but close enough to cause potential complications in vaginal delivery.
Partial placenta previa
The placenta partially covers the cervix with varying extents of coverage.
Complete placenta previa
In complete placenta previa, the placenta completely covers the cervical opening. It comes with a high bleeding risk and usually requires cesarean delivery.
What causes placenta previa?
Risk factors for developing placenta previa include:
- Prior placenta previa
- Prior cesarean section
- Other prior uterine surgery
- Assisted reproductive technology
- Uterine fibroids
- Multiple gestation
- Advanced maternal age
- Grand multiparity
- Smoking
- Cocaine use
Placenta previa treatments and diagnosis: dos and don’ts for nurses
If previa is already diagnosed (identified on an early pregnancy ultrasound):
- Evaluate for placenta accreta.
- Monitor placental location with serial ultrasounds.
- If previa is persistent, a cesarean will need to be planned at 36 to 37 weeks.
If a client presents with vaginal bleeding in the second or third trimester:
- Previa should be excluded or diagnosed with an ultrasound assessment.
- Evaluate for placenta accreta.
- Initiate serial vital signs and electronic fetal monitoring.
- Insert two large-bore intravenous lines.
- Labs: CBC, coags, type/screen, Kleihauer–Betke test
- Consider steroids for fetal lung maturation and magnesium sulfate for neuroprotection, depending on gestational age and severity of bleeding.
- Cesarean delivery, if severe/persistent bleeding
- May consider expectant management if bleeding subsides and both client and fetal status remain reassuring
Avoid vaginal exams on any pregnant client with vaginal bleeding until placental location is confirmed. Exam may disrupt placenta and worsen bleeding.
Outside of bright red, painless vaginal bleeding in the second or third trimester, placenta previa can present with:
- Soft, non-contractile uterus
- Fetal distress (if placental perfusion compromised by severe bleeding)
- Client with signs of shock (due to severe bleeding)
Vasa previa vs placenta previa
Vasa previa and placenta previa are both obstetric complications, but they are different conditions. Both have a potentially dangerous loss of blood as their main risk. The key difference is that placenta previa involves the placement of the placenta itself, while vasa previa involves the placement of fetal blood vessels.
Placenta previa involves the placenta covering or being near the cervix. Vasa previa occurs when fetal blood vessels from the umbilical cord or placenta cross the entrance to the birth canal beneath the fetus.
Placenta previa self-care: patient education
Clients should be advised to:
- Seek medical attention immediately for any episode of vaginal bleeding!
- Understand the importance of pelvic rest: Avoid placing anything in the vagina, as that may disrupt the placenta. This includes vaginal exams by providers before the placental location is confirmed.