Types of pain
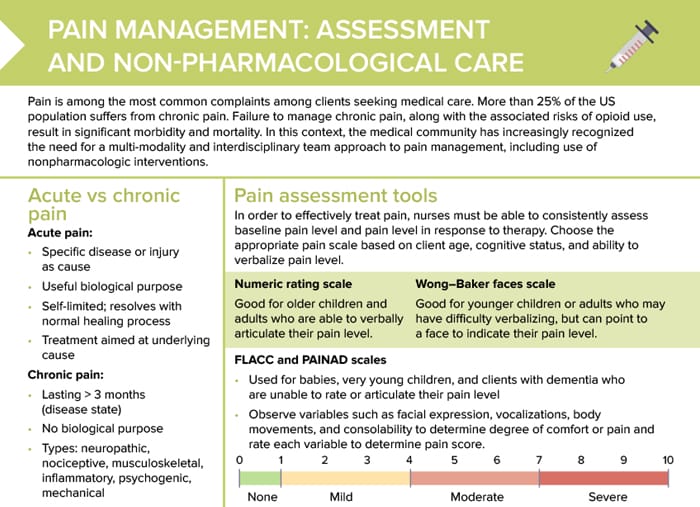
Pain is among the most common reports among clients/patients seeking medical care. Pain can be acute or chronic.
Acute pain
Acute pain is due to a specific disease or injury. It has a useful biological purpose and is self-limited, resolving with the natural healing process. The treatment is aimed at the underlying cause.
Chronic pain
Chronic pain is defined as pain lasting more than 3 months. It has no biological purpose and comes with an increased risk of anxiety, depression, and suicidality. Most clients report more than one type of chronic pain: neuropathic, nociceptive, musculoskeletal, inflammatory, psychogenic, mechanical.
Research shows about 25% of the US population suffers from chronic pain. Failure to manage chronic pain, along with the associated risks of opioid use, result in significant morbidity and mortality.
Pain scales for assessment
In order to effectively treat pain, nurses must be able to consistently assess baseline pain level and pain level in response to therapy. Choose the appropriate pain scale based on client age, cognitive status, and ability to verbalize pain level.
Pain scale: “1–10” (numeric)
Useful for older children and adults who are able to verbally articulate their pain level, rating pain on a numeric scale from 1 to 10 is a simple and effective way to determine pain intensity.
Pain scale: “FACES®” (Wong–Baker)
In the Wong–Baker FACES® scale, the client is presented with a visual scale with happy or increasingly distressed-looking faces that indicate pain intensity. The client then points to a face that indicates their pain level, making this method useful for younger children or adults who may have difficulty verbalizing.
CPOT pain scale
The CPOT (critical-care pain observation tool) pain scale was developed for assessing pain in critically ill patients who are unable to communicate. It rates 4 behavioral indicators: facial expressions, body movements, muscle tension, and compliance with the ventilator or vocalization in non-intubated patients.
McGill pain scale
The McGill pain questionnaire is used for individuals who are able to communicate verbally. It assesses pain using descriptors grouped into 20 categories, providing a very in-depth, detailed description of the patient’s experience.
PAINAD/FLACC pain scales
The FLACC (face, legs, activity, cry, consolability) and PAINAD (pain assessment in advanced dementia) scales are used for babies, very young children, and clients with dementia who are unable to rate or articulate their pain level. The nurse observes variables such as facial expression, vocalizations, body movements, and consolability to determine degree of comfort or pain and rates each variable to determine pain score.
PQRST pain assessment
The PQRST method provides a comprehensive understanding of a client’s pain experience, not only looking at pain severity, but also other factors:
- Provocation/palliation (what makes the pain better or worse)
- Quality (sharp, throbbing)
- Region (location, radiation)
- Severity
- Timing (constant, intermittent)
Pain: nursing diagnosis
Pain as a nursing diagnosis is a recognition by nurses that a patient is experiencing discomfort or distress.
Pain as a nursing diagnosis can be further categorized and defined in various ways:
- Acute pain
- Chronic pain
- Activity intolerance related to pain
- Ineffective coping related to pain
When formulating a nursing diagnosis for pain, the nurse should be as specific as possible regarding:
- Location of the pain
- Characteristics of the pain (sharp, dull, stabbing)
- Severity, often on a scale from 0 to 10
- Onset, duration, and any known or perceived cause
- Any associated symptoms or aggravating/relieving factors
Once the nursing diagnosis is established, it guides the formulation of care plans to manage and alleviate the pain.
Nonpharmacologic pain management strategies
- Heat or cold therapy
- Hydrotherapy
- Distraction or companionship
- Transcutaneous electrical nerve stimulation
- Relaxation
- Counseling or pastoral services
- Meditation
- Alternative and complementary medicine