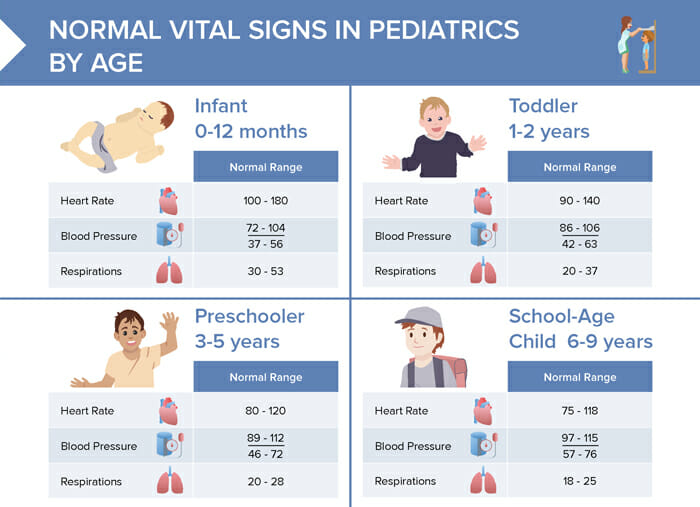
What are normal vital signs for infants (0–12 months)?
- Heart rate: 100–180
- Blood pressure: 72–104/37–56
- Respiration: 30–53
What are normal vital signs for toddlers (1–2 years)?
- Heart rate: 90–140
- Blood pressure: 86–106/42–63
- Respiration: 20–37
What are normal vital signs for preschoolers (3–5 years)?
- Heart rate: 80–120
- Blood pressure: 72–104/46–72
- Respiration: 20–28
What are normal vital signs for school-aged children (6–9 years)?
- Heart rate: 75–118
- Blood pressure: 97–115/57–76
- Respiration: 18–25
What are normal vital signs for adolescents (10–15 years)?
- Heart rate: 60–100
- Blood pressure:
- 10–12 years: 102–120/61–80
- 13–15 years: 110–131/64–83
- Respiration: 12–20
How to take vital signs in children
While the process of taking vital signs consists of very similar steps to taking vital signs in adults, there are additional considerations when caring for children. They are smaller and may be distressed/crying in a clinical environment. If children are scared, it can help to show the equipment, explain what you’re going to do, or use distractions like a toy or video.
- Temperature:
- Rectal: most accurate
- Axillary
- Oral: for older children who can hold the thermometer under their tongue
- Tympanic or temporal artery: quickly swipe across forehead or place in ear → reduced distress
- Pulse:
- For infants, use the brachial or apical pulse
- For older children, the radial pulse is usually fine
- Count the pulse for a full minute to ensure accuracy, especially as children’s heart rates can be irregular
- Respiration: Without letting the child know you’re counting their breaths (as this can alter their breathing rate), count the number of breaths for one minute. Watch for the rise and fall of the chest or abdomen.
- Blood pressure: Use an appropriately-sized cuff (about 40% of the circumference of the arm). Check blood pressure last; if needed, leave cuff on and return to check later when child is calm.
- Oxygen saturation (SpO2): Make sure the pulse oximeter is sized appropriately for the child.
- Pain: Use an age-appropriate pain scale (like the “FACES” scale for younger children) to assess if the child is in pain.