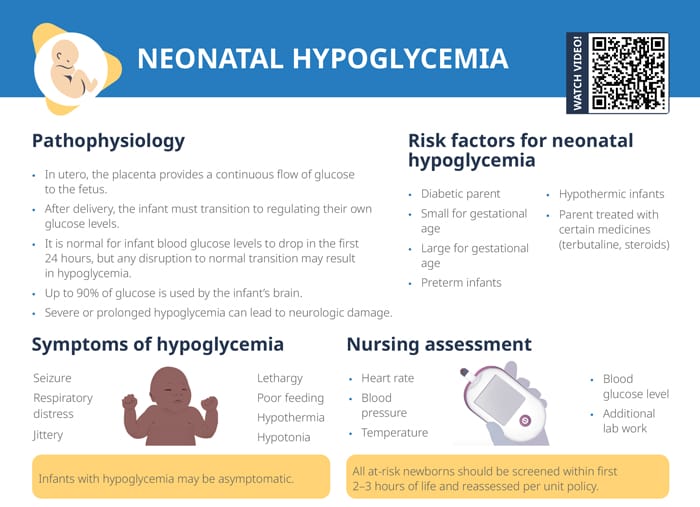
What is neonatal hypoglycemia?
- In utero, the placenta provides a continuous flow of glucose to the fetus.
- After delivery, the infant must transition to regulating their own glucose levels.
- It is normal for infant blood glucose levels to drop in the first 24 hours, but any disruption to normal transition may result in hypoglycemia.
- Up to 90% of glucose is used by the infant’s brain.
- Severe or prolonged hypoglycemia can lead to neurologic damage.
Risk factors and causes of neonatal hypoglycemia
Risk factors that make it more likely an infant might become affected by hypoglycemia include:
- Diabetic parent
- Small or large for gestational age
- Preterm
- Hypothermic
- Parent treated with certain medicine (terbutaline, steroids)
Which medication is responsible for neonatal hypoglycemia?
The parent being treated with certain kinds of medications can increase the risk for neonatal hypoglycemia in the infant, including:
- Insulin or other hypoglycemic medications
- Beta-blockers (atenolol, propranolol)
- Indomethacin (pain reliever)
- Terbutaline
- Steroids
Symptoms of neonatal hypoglycemia
Look for the following symptoms in infants:
- Seizures
- Respiratory distress
- Jittery
- Lethargy
- Poor feeding
- Hypothermia
- Hypotonia
Note that infants with hypoglycemia may be asymptomatic.
Infant nursing assessment
Measure infant:
- Heart rate
- Blood pressure
- Temperature
- Blood glucose level
- Additional lab work
All at-risk newborns should be screened within the first 2–3 hours of life and reassessed per unit policy.
Neonatal hypoglycemia treatment
Interventions are:
- Feed infant
- Dextrose gel
- IV glucose
Always reassess blood glucose levels 20–30 minutes after intervention.
Management according to severity of hypoglycemia:
- Blood glucose below 20: intervene with fast-acting glucose
- Blood glucose 20–40: feed infant (if able to and delivered at term)
- Blood glucose over 40: normal care
Always check the unit’s specific policy for treatment levels.