What is multiple sclerosis (MS)?
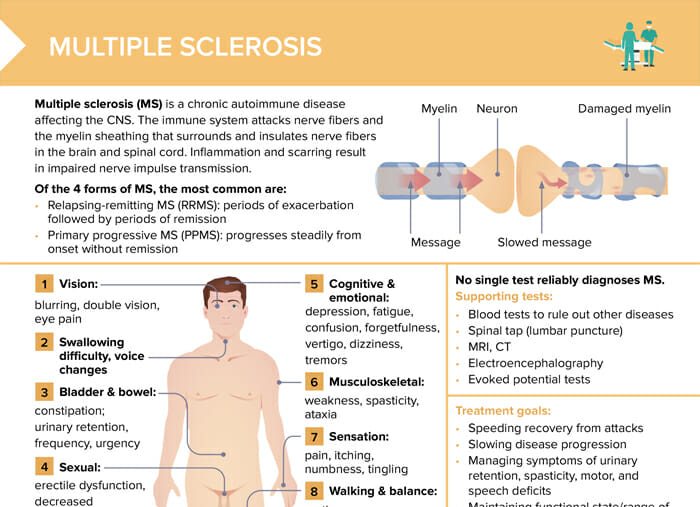
Multiple sclerosis (MS) is a chronic autoimmune disease affecting the CNS. The immune system attacks nerve fibers and the myelin sheathing that surrounds and insulates nerve fibers in the brain and spinal cord. Inflammation and scarring result in impaired nerve impulse transmission.
What causes MS?
The cause of MS is not entirely known, and it’s likely influenced by a combination of genetic and environmental factors.
What are usually the first signs of MS?
The first signs of multiple sclerosis (MS) can vary greatly among individuals because the location and severity of each attack can differ. Common initial symptoms include:
- Optic neuritis (partial or complete loss of vision usually in one eye at a time, often with pain during eye movement)
- Swallowing/voice changes
- Tingling or numbness in the face, body, or extremities
- Weakness/fatigue
- Problems with balance or coordination, tremors
- Dizziness or vertigo
- Bladder or bowel issues (frequency, urgency, or retention)
- Pain or muscle spasticity
Forms of MS: how does multiple sclerosis progress?
Over time, the disease can cause the nerves themselves to deteriorate or become permanently damaged. As the disease progresses, individuals with MS may experience increased difficulty with walking and mobility, greater levels of fatigue, more problems with balance and coordination, and increased cognitive, bowel, and bladder issues. However, the progression of MS is highly individual, and not everyone will experience all symptoms or the same level of disability.
MS forms can be categorized according to their patterns of symptoms in disease progression:
- Relapsing-remitting MS (RRMS):
- Most common disease course
- Characterized by clear episodes of neurological symptoms (relapses) followed by periods of partial or complete recovery (remissions)
- Symptoms may be active, then improve or disappear for months or even years, but then come back or worsen
- Primary-progressive MS (PPMS):
- Characterized by a gradual worsening of neurological function without any distinct relapses or remissions
- Temporary minor improvements or plateaus where symptoms remain stable for a time
- Secondary-progressive MS (SPMS):
- Initially begins as RRMS
- Transitions into a phase characterized by a steady worsening of neurological function, similar to PPMS
- Occasional relapses, minor remissions, or plateaus are possible
- Progressive-relapsing MS (PRMS):
- Relatively rare
- Characterized by a steady worsening of disease from the onset but with clear superimposed relapses
- Recovery following these relapses is possible
Does MS affect life expectancy?
Most people affected by MS have a normal or near-normal life expectancy; however, complications from severe MS may affect life expectancy (e.g. infections).
How is MS diagnosed?
No single test reliably diagnoses multiple sclerosis.
Supporting tests:
- Blood tests to rule out differential diagnoses
- Spinal tap (lumbar puncture)
- MRI, CT
- Electroencephalography
- Evoked potential tests
Multiple sclerosis: treatment
There is no cure for MS. Management of multiple sclerosis aims to slow disease progression, speed up recovery from attacks, maintain functional state/range of motion and emotional/mental health, and improve quality of life by addressing symptoms.
- Medical treatment to slow progression and reduce severity/frequency of relapses:
- Corticosteroids, immunomodulators, interferons, immunoglobulins, monoclonal antibodies, chemotherapy agents
- Symptomatic treatment:
- Drugs for fatigue, depression, pain, muscle spasticity, sexual dysfunction, insomnia, bladder and bowel problems, increased walking speed
- Patient education:
- Avoid fatigue, stress, infection, overheating, chilling.
- Balance moderate exercise with rest.
- Maintain regular bowel and bladder elimination.
- Eat a balanced diet and increase fluid intake.
- Adopt safety measures to reduce injury related to motor/sensory loss.
- Notify provider of any exacerbation or worsening of condition.
How can nurses support MS patients in managing their symptoms and maintaining quality of life?
- Ensure patient education on disease and management (advice on medications, provide resources for lifestyle modifications)
- Facilitate coordination with rehabilitation therapists and mental health professionals
- Assist in managing symptoms
Multiple sclerosis nursing diagnoses
Potential nursing diagnoses of MS:
- Impaired physical mobility: encourage physical activity, refer to physiotherapy
- Fatigue: educate client about energy conservation techniques and balanced diet
- Disturbed sensory perception: educate on assistive devices, teach family to monitor changes, ensure safe environment
- Bowel/urinary incontinence: encourage adequate hydration, advise on fiber-rich diet, bladder training
- Ineffective coping/deficient knowledge: educate client on MS, refer to counseling or support groups, provide emotional support
How does MS typically present in pediatric clients compared to adults?
While MS is typically diagnosed in adults, it can also occur in children and adolescents. Pediatric MS might present similarly to adult MS with symptoms such as numbness, tingling, weakness, imbalance, vision problems, and fatigue. However, children may have additional challenges, including seizures and prominent cognitive issues, which can affect school performance and social development. They might also have a higher relapse rate than adults with MS, but they tend to recover better from each relapse. Pediatric MS requires a specialized approach to care, addressing not only the physical symptoms but also the developmental, educational, and psychosocial aspects.