Nursing Knowledge
Lithium is the third element on the periodic table and the oldest mood-stabilizing drug. It is used to treat bipolar disorder, schizophrenia, and borderline personality disorder.
Lithium is taken orally in pill, capsule, or liquid form. Dosing is titrated based on desired effect and serum level monitoring. It usually takes 5–7 days from initiation of therapy to note benefit and up to 3 weeks to achieve peak effect.
While the exact mechanism of action is unknown, lithium modifies sodium transport in nerve and muscle cells, is thought to alter the metabolism of neurotransmitters (specifically catecholamines and serotonin), and may alter intracellular signaling.
Lithium has a narrow therapeutic window and can cause significant adverse effects. Careful monitoring is required.
*Lithium is a positively-charged ion and is processed like sodium by the kidneys. Low serum Na+ causes the kidneys to retain Li+ along with sodium. Li+ retention can lead to toxicity.
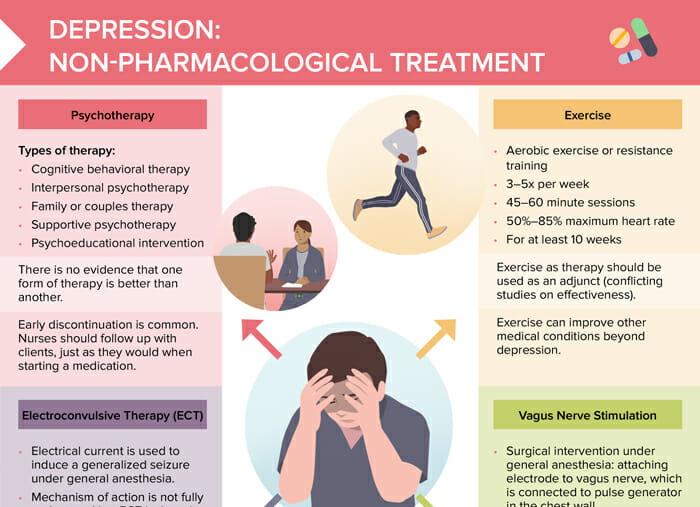
Review of non-medication treatment options for depression
RELATED TOPIC:
Free Download
Master the topic with a unique study combination of a concise summary paired with video lectures.
USMLE™ is a joint program of the Federation of State Medical Boards (FSMB®) and National Board of Medical Examiners (NBME®). MCAT is a registered trademark of the Association of American Medical Colleges (AAMC). NCLEX®, NCLEX-RN®, and NCLEX-PN® are registered trademarks of the National Council of State Boards of Nursing, Inc (NCSBN®). None of the trademark holders are endorsed by nor affiliated with Lecturio.
Your free account gives you access to:
or
Have a holly, jolly study session 🎁 Save 50% on all plans now >>