What is gestational diabetes?
Gestational diabetes is a type of diabetes that occurs during pregnancy. It can occur at any stage of pregnancy but is more common in the second or third trimester, and often resolved on its own after birth.
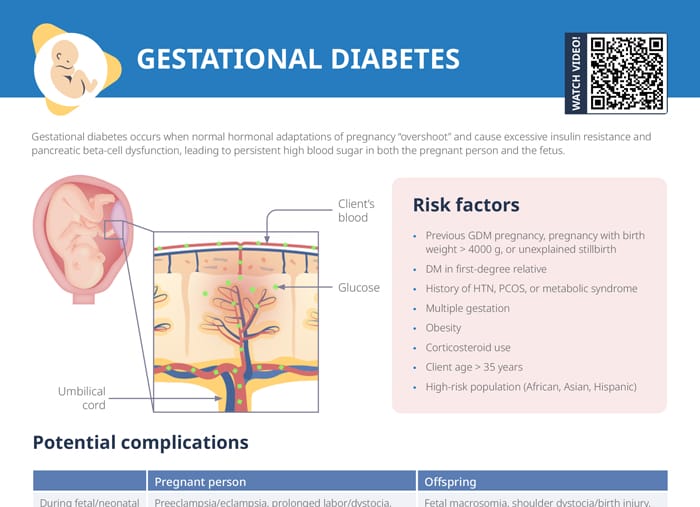
Gestational diabetes is caused by normal hormonal adaptations of pregnancy “overshooting” and causing excessive insulin resistance and pancreatic beta-cell dysfunction, which lead to persistent high blood glucose in both the pregnant person and the fetus.
Related videos
What causes gestational diabetes?
Risk factors for developing diabetes in pregnancy
- Previous GDM pregnancy, pregnancy with birth
- Weight > 4000 g, or unexplained stillbirth
- DM in first-degree relative
- History of HTN, PCOS, or metabolic syndrome
- Multiple gestation
- Obesity
- Corticosteroid use
- Client age > 35 years
- High-risk population (African, Asian, Hispanic)
Screening and diagnosis
For most pregnant clients, a 2-step screening process is used:
- 1-hour glucose tolerance test (GTT) at 24–28 weeks
- Follow up with 3-hour GTT if glucose elevated on 1 hour
Postpartum, a 2-hour GTT at 6–12 weeks is recommended, as well as follow-up tests every 3 years for detection of DM II.
Home glucose monitoring
Clients diagnosed with GDM should monitor blood glucose upon waking each morning and after each meal, and for the remainder of the pregnancy.
How is gestational diabetes treated?
The main treatment goals are maintaining euglycemia and preventing complications.
First-line therapy
Measures affecting diet and exercise are the first recommendations to clients to control gestational diabetes:
- Nutritional counseling
- Personalized meal plan
- 30 min/day exercise at least 5 days/week
- Moderate-intensity cardio, plus light weight training
Further interventions (if lifestyle changes ineffective)
If no adequate glycemic control can be achieved with lifestyle modifications, further measures are insulin therapy (personalized dose subQ self-injection) and oral hypoglycemics (glyburide and metformin increasingly prescribed while no oral agent currently FDA-approved for use in GDM).
Possible complications of gestational diabetes
- Possible complications during GDM pregnancy: preeclampsia, eclampsia, prolonged labor/dystocia, Cesarean delivery, surgical complications, postpartum hemorrhage
- Complications affecting the fetus: fetal macrosomia, shoulder dystocia/birth injury, polycythemia, neonatal hypoglycemia, respiratory distress syndrome, jaundice, perinatal mortality
- Long-term increased risks for both parent and baby:
- Obesity
- DM II (or I in baby)
- Cardiovascular disease
- For pregnant person only: renal disease and malignancies
How to prevent gestational diabetes
While some risk factors for gestational diabetes cannot be influenced by the client and prevention can never be guaranteed, some strategies can help reduce the risk:
- Maintaining a healthy weight
- Eating a balanced diet
- Following a consistent exercise routine
- Monitoring blood glucose levels and following the medical check-up schedule
Nursing diagnoses for gestational diabetes
Possible nursing diagnoses for clients with gestational diabetes include:
- Risk for fetal injury due to complications from high blood glucose levels (macrosomia, birth trauma, neonatal hypoglycemia) → monitor levels
- Imbalanced nutrition (more than body requirements): Condition may be exacerbated by inappropriate diet → provide counseling and monitor weight gain
- Deficient knowledge
- Anxiety
- Risk for ineffective health maintenance due to problems with lifestyle changes and treatment plan → assist in setting feasible goals and provide resources
Gestational diabetes meal plan advice for clients
When creating meal plans for clients with gestational diabetes, the focus should be on balancing carbohydrates with protein and healthy fats to help control blood glucose levels.
Gestational diabetes recipes
General guidelines when meal-planning with gestational diabetes include including protein, healthy fats, and moderate amounts of complex carbohydrates in each meal. Portion control, staying well-hydrated, and keeping regular intervals for meals should be recommended as well.
Some examples of meals that fit these requirements for inspiration include:
- Grilled fish with steamed vegetables and quinoa
- Tofu stir-fry with bell peppers and carrots over a small portion of brown rice
- Lentil soup with a side of whole-grain bread
- Grilled chicken salad, whole-grain bread optional
- Scrambled eggs with spinach and whole-grain toast
Gestational diabetes snacks
Foods to avoid with gestational diabetes are processed foods or those with high sugar content. Suitable snacks include:
- Nuts such as almonds, pumpkin seeds, or walnuts
- Raw vegetables with a dip (hummus or greek yogurt)
- Hard-boiled eggs
- Roasted chickpeas
- Edamame