What is episiotomy?
An episiotomy is a procedure where a surgical incision is made to widen the vaginal opening. It is typically performed during labor to facilitate the delivery of the infant.
Episiotomies are no longer performed routinely or without indication. Rates of episiotomies are declining.
Episiotomy vs tearing
The tissues around the vaginal opening may tear during childbirth due to the baby’s head and body stretching the tissues. Depending on the degree of tearing, surgical repair may be needed. Natural tearing may heal better than making an intentional incision, and the decision will be made for the client individually if episiotomy is likely to lead to a better outcome.
Related videos
Indications
Episiotomy is indicated:
- When expedite delivery of the infant is needed
- Operative delivery
- To reduce vaginal tearing
- To reduce trauma to the infant (e.g., shoulder dystocia)
- If the client has a history of female genital mutilation or cutting
Risks of episiotomy
Cutting the tissues around the vaginal opening comes with several risks:
- Extension of the incision (3rd- or 4th-degree tear)
- Bleeding
- Infection, dehiscence
- Poor healing (fistula, narrowing of introitus)
- Perineal pain, dyspareunia
Clients should be educated that episiotomy increases the risk of severe lacerations in subsequent deliveries.
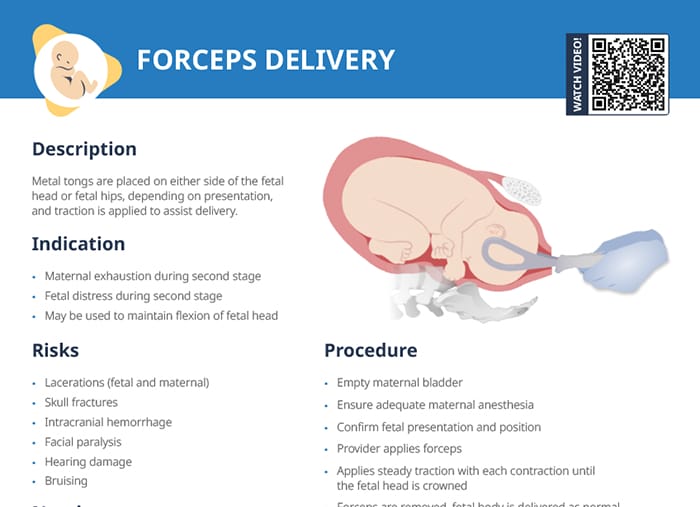
4 types of episiotomy
Midline episiotomy
Midline episiotomies are the most common type of episiotomy performed in the US. A straight incision is made from the posterior vaginal opening toward the anus. They are easy to repair, however, they increase the risk of 3rd- or 4th-degree lacerations.
Mediolateral episiotomy
This incision begins at the same point as the midline episiotomy, but is angled away from the rectum. In a mediolateral episiotomy, the risk of blood loss is increased, but the risk of 3rd- or 4th-degree laceration is not impacted.
Midline and mediolateral episiotomies are the most commonly performed. The selection between the two depends on several factors including the anticipated size of the baby, position during delivery, and the likelihood of tissue tearing naturally.
Lateral episiotomy
A lateral episiotomy is similar to mediolateral, but the incision is made farther to the side. This type is rarely used because the risk of bleeding and nerve damage is higher with this variation.
J-shaped episiotomy
This is a variation where the incision starts like a midline but curves away from the anus in a ‘J’ shape to reduce the risk of extending to the anal sphincter.
Procedure and nursing care
The procedure is performed by a provider, at the time when the delivery of the fetal head is imminent. Nursing tasks include monitoring, comforting the patient, and advocating for the client in terms of education and pain control:
- Comfort care, including perineal ice packs and peri-bottle
- Monitor for bleeding and hematoma formation postpartum
- Monitor for signs of infection
- Monitor for wound dehiscence
Procedure steps:
- Obtain informed verbal consent
- Ensure adequate anesthesia
- Fetal head is protected by provider’s fingers
- Starting at introitus, either a lateral or medial incision is made by scalpel or surgical scissors
- Support perineum through delivery of fetal head to reduce risk of extension
- Following delivery: thorough examination of perineum and rectum
- Surgical repair of the incision
Episiotomy healing
Healing from an episiotomy typically begins immediately after childbirth, with the incision usually sutured by the healthcare provider using absorbable stitches. The initial healing phase, where the surface tissues begin to heal, typically lasts for about 2-3 weeks. Complete internal healing can take up to 6 weeks or longer.
After delivery, encourage stool softeners, fluids, and a high-fiber diet to prevent straining with bowel movements. Advise clients to avoid strenuous activity and lifting heavy objects during healing. Discuss resuming sexual activity based on the client’s comfort and healing.
- Pain management: NSAIDs commonly recommended
- Hygiene: gently clean area with warm water, pat dry; sitz baths
- Monitoring for infection
Scarring and complications
- Pelvic floor exercises can be beneficial once comfortable to strengthen muscles
- Scar massage (once healed) can help prevent tissue adhesion and reduce scar formation
- Give options for persistent pain or discomfort, e.g. referral to pelvic health therapist
- Clients should be educated on the signs of infection and contact the provider immediately.