What does a normal sinus rhythm look like?
In a normal sinus rhythm, an electrical impulse originates from the SA node in the right atrium and travels to the ventricles via the AV node and His-Purkinje system, producing a regular rhythm and heart rate between 60–100 beats per minute.
What is dysrhythmia?
Dysrhythmia, or arrhythmia, is an abnormal or irregular heart rhythm resulting from disruptions in the heart’s electrical conduction system.
How are dysrhythmias detected?
Electrocardiograms (ECG/EKG) and telemetry are commonly used for continuous monitoring of heart rhythms.
Early detection of dysrhythmias can prevent complications, such as heart failure, stroke, or sudden cardiac death.
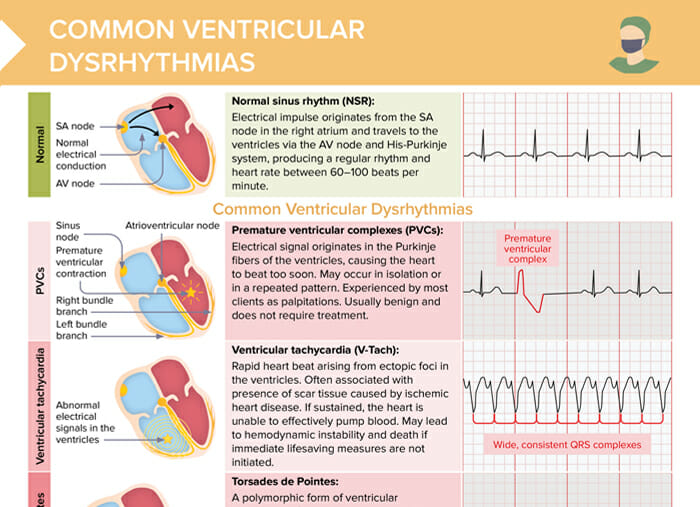
Common ventricular dysrhythmias
Free download:
Overview of common ventricular dysrhythmias, cardiac conduction patterns, and associated ECG changes
Premature ventricular complexes (PVC)
- Electrical signal originates in the Purkinje fibers of the ventricles, causing the heart to beat too soon
- May occur in isolation or in a repeated pattern
- Experienced by most clients as palpitations
- Usually benign and does not require treatment
Ventricular tachycardia (V-Tach)
- Rapid heart beat arising from ectopic foci in the ventricles
- Often associated with presence of scar tissue caused by ischemic
- heart disease
- If sustained, the heart is unable to effectively pump blood
- May lead to hemodynamic instability and death if immediate lifesaving measures are not initiated.
Torsades de Pointes
- A polymorphic form of ventricular tachycardia
- Characterized by oscillatory changes in amplitude of QRS complexes around the isoelectric line on ECG/EKG
- Results from congenital or acquired QTc prolongation
- Torsades may resolve spontaneously or may degenerate into ventricular fibrillation. May respond to Mg infusion
Ventricular fibrillation (V-Fib)
- Irregular electrical activity originating from multiple sites within the ventricles
- Usually associated with underlying structural heart disease
- The ventricles quiver instead of pumping blood, which decreases cardiac output and can be fatal within minutes without intervention.
- Present in 70% of sudden cardiac deaths
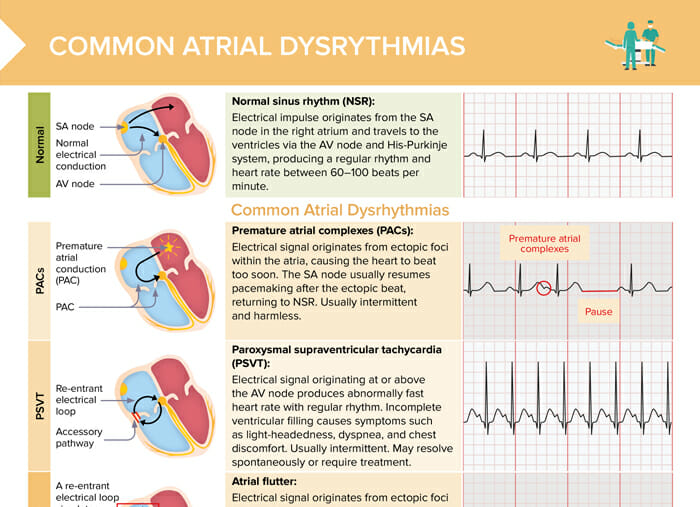
Common atrial dysrhythmias
Premature atrial complexes (PACs)
- Electrical signal originates from ectopic foci within the atria, causing the heart to beat too soon.
- The SA node usually resumes pacemaking after the ectopic beat, returning to NSR.
- Usually intermittent and harmless
Paroxysmal supraventricular tachycardia (PSVT)
- Electrical signal originating at or above the AV node produces abnormally fast heart rate with regular rhythm
- Incomplete ventricular filling causes symptoms such as light-headedness, dyspnea, and chest discomfort
- Usually intermittent
- May resolve spontaneously or require treatment
Atrial flutter
- Electrical signal originates from ectopic foci in the atria and travels through a reentry pathway, causing the atria to beat at a rate 3–4 times that of the ventricles.
- On ECG, atrial flutter is recognized via a characteristic “saw tooth” pattern.
- Puts clients at risk for blood clots and stroke
- Must be treated
Atrial fibrillation (A-fib)
- Multiple ectopic foci in the atria fire rapidly, producing a fast, uncoordinated atrial rhythm with irregular ventricular response.
- Insufficient ventricular filling can cause symptoms such as fatigue, light-headedness, SOB, and chest discomfort.
- Turbulent flow of blood through the atria puts clients at risk for blood clots and stroke.
- Must be treated
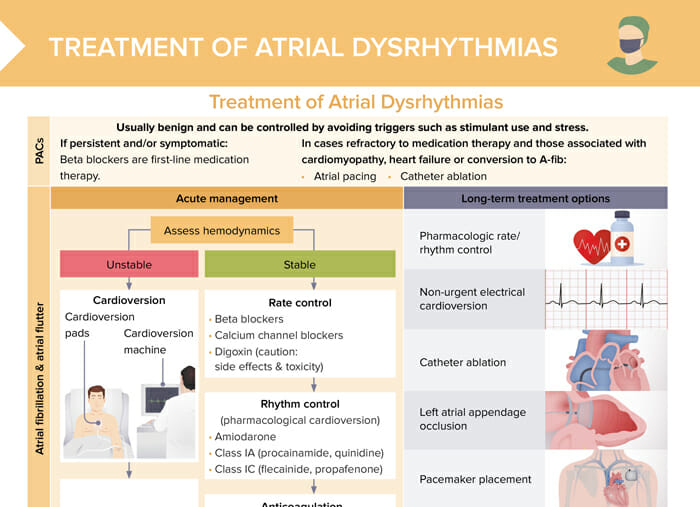
Treatment of atrial dysrhythmias
Atrial dysrhythmias are usually benign and can be controlled by avoiding triggers such as stimulant use and stress. If they are persistent or symptomatic, beta blockers are the first-line medication therapy. In cases refractory (unmanageable) to medication therapy and those associated with cardiomyopathy, heart failure, or conversion to A-Fib, options include atrial pacing and catheter ablation.
Free download:
Overview of acute and long-term treatment options for atrial dysrhythmias
Acute management of atrial fibrillation and atrial flutter
Assess hemodynamics:
- If stable:
- Rate control (beta blockers, calcium channel blockers, digoxin)
- Rhythm control (amiodarone, class IA, class IC)
- Anticoagulation (based on stroke risk stratification using a scoring system such as CHADS2-Vasc)
- If unstable:
- Cardioversion
- Anticoagulation for stroke prevention
Long-term treatment options for atrial fibrillation and atrial flutter
- Pharmacologic rate/rhythm control
- Non-urgent electrical cardioversion
- Catheter ablation
- Left atrial appendage occlusion
- Pacemaker placement
- Anticoagulation
Acute management of PSVT
Assess hemodynamics:
- If stable:
- Attempt valsalva maneuver
- If SVT persists, adenosine rapid IV push (momentarily stops heart and may allow it to restart in normal sinus rhythm)
- If unstable: cardioversion
Long-term treatment options for PSVT
- Maintenance medications: beta blockers, calcium channel blockers
- Override pacing: pacing heart at faster rate than native rhythm may help discontinue SVT
- Catheter ablation