What is a chest tube?
A chest tube, also known as a thoracic catheter, is a flexible plastic tube that is inserted through the chest wall and into the pleural space or mediastinum.
What is the purpose of a chest tube?
The purpose of a chest tube is to remove air (pneumothorax), fluid (pleural effusion, hemothorax), or pus (empyema) from the intrathoracic space. This is a critical procedure in managing conditions such as pneumothorax or pleural effusion where the accumulation of air or fluid in the pleural space can compromise lung function. It is also used after cardiothoracic surgery to re-expand the lungs.
How is a chest tube used?
The chest tube is usually connected to a chest drain system that allows the removal of air or fluid and prevents a return of air/fluid to the pleural space. The chest drain system can either be a wet (water seal) or dry system.
The procedure to insert a chest tube is done under sterile conditions and usually under local anesthesia. It’s a common procedure but not without risks, and is typically performed in a hospital setting.
Related videos
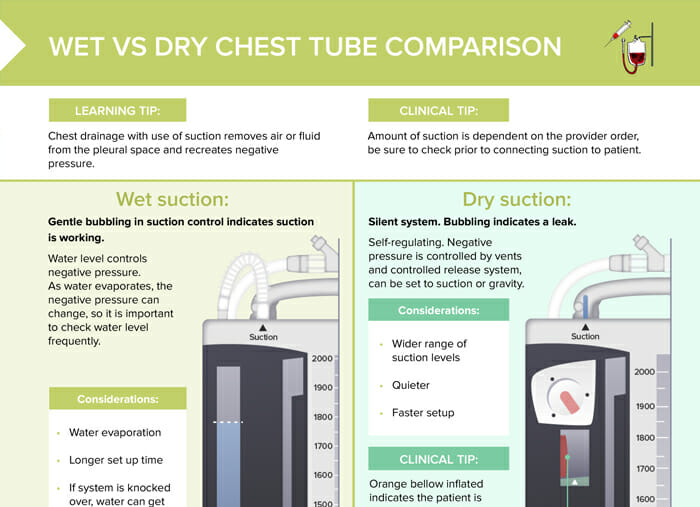
Wet vs dry suction: comparison of similarities and differences
Wet and dry suction refer to two different types of chest drainage systems used in conjunction with a chest tube. Both systems serve the same purpose: to remove air, fluid, or blood from the pleural space and to prevent these substances from returning to the chest.
The most important difference between wet and dry chest tube suction lies in the mechanisms of creating negative pressure: wet suction uses a column of water to regulate negative pressure, while dry suction uses a mechanical regulator. Additionally, wet suction systems require frequent monitoring of water levels due to evaporation, while dry suction systems are self-regulating, generally quieter and faster to set up.
How does wet suction work?
In a wet suction system, the water level controls the negative pressure. As water evaporates, the negative pressure can change, so it’s important to check the water level frequently. The amount of suction (e.g., -20 cm H2O) is indicated by the water level. Gentle bubbling in the suction control indicates that the suction is working.
Considerations for wet suction include:
- Water evaporation can affect the negative pressure.
- It has a longer setup time compared to dry suction.
- If the system is knocked over, water can get into other chambers, potentially compromising the system.
How does dry suction work?
In a dry suction system, the negative pressure is self-regulating and is controlled by vents and a controlled release system. This system can be set to suction or gravity. An orange bellow inflated indicates that the client is connected to suction, and the suction is controlled by a dial. Unlike the wet suction system, the dry suction system is silent, and any bubbling indicates a leak.
Considerations for dry suction include:
- It offers a wider range of suction levels.
- It is quieter than the wet suction system.
- It has a faster setup time.
The amount of suction is dependent on the provider’s order, so it’s important to check this prior to connecting suction to the client.
What are the clinical safety tips related to the use of chest tubes?
- Never lift the drain above chest level: This is crucial to prevent backflow and maintain the effectiveness of the suction.
- Check the water level frequently in wet suction: As water evaporates, the negative pressure can change, affecting the effectiveness of the suction.
- Be careful not to knock over the system: In a wet suction system, if the system is knocked over, water can get into other chambers, potentially compromising the system.
- Check the provider’s order for the amount of suction: The amount of suction is dependent on the provider’s order, so it’s important to check this prior to connecting suction to the client.
- Monitor for air leaks: Both wet and dry suction systems have air leak chambers. Higher numbers in these chambers indicate worsening air leaks.