What is bipolar disorder?
Bipolar disorder is a mental health condition characterized by extreme mood swings that can range from manic highs to depressive lows. It is a mood disorder that affects millions of people worldwide and can interfere with daily life, relationships, and work.
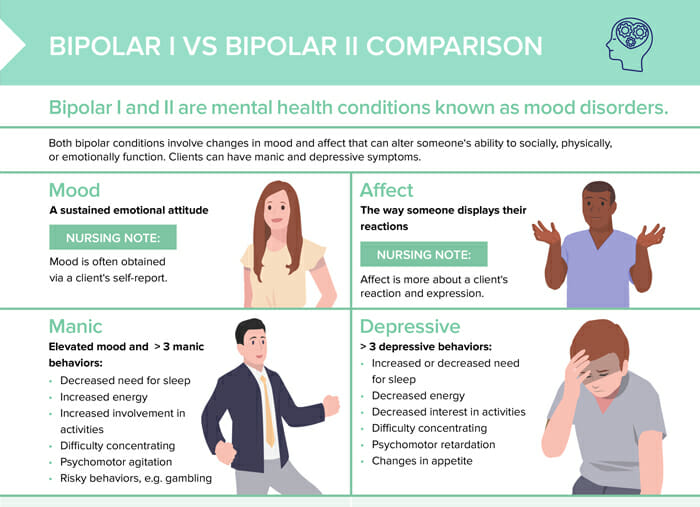
A client’s ‘mood’ can be described as their sustained emotional attitude, while ‘affect’ references the way someone displays their emotions.
Note: Mood is often obtained via a client’s self-report. Affect is more about a client’s reaction and expression.
How common is bipolar disorder?
Bipolar disorder affects approximately 2.8% of the adult population worldwide. Bipolar I is equally seen in men and women, while bipolar II is more common in women.
Is bipolar a personality disorder?
Bipolar disorder is not categorized as a personality disorder, but as a mood disorder. Personality disorders typically involve ongoing changes in thoughts and behavior, while bipolar is characterized by episodic mood changes.
Is bipolar disorder genetic?
Bipolar disorder is thought to have a genetic component as one of several factors that can influence its onset, including environmental factors and life events.
When was bipolar disorder discovered?
Around the 1st century AD, a Greek physician observed patients who would cycle between mania and depression. However, the modern understanding of bipolar disorder began in the 19th century with French psychiatrist Jean-Pierre Falret describing “circular insanity” (folie circulaire) in 1851, noting the alternation between manic and depressive episodes. This laid the foundation for our contemporary understanding of the disorder.
Types of bipolar disorder: comparison
Bipolar I
Bipolar I is defined by at least 1 manic episode and 1 major depressive episode. It is equally seen in men and women.
Bipolar II
Bipolar II is characterized by at least 1 depressive episode lasting at least 2 weeks and at least 1 hypomanic episode.
Nursing diagnosis for bipolar disorder
When caring for patients with bipolar disorder, nurses might identify several potential nursing diagnoses based on the patient’s presentation and needs. Here are some common ones:
- Ineffective activity planning: related to hallucinations or delusions, misperception of events and information
- Fatigue: sleep deprivation related to manic hyperactivity or insomnia, psychological demands
- Ineffective health management: also imbalanced nutrition (less than body requirements) related to lack of time and good judgment/getting help
- Risk-prone health behavior: noncompliance with medication regimen due to side effects, denial, low optimism
- Ineffective coping
Symptoms of bipolar disorder
Symptoms of mania and hypomania
- Increased energy and activity
- Elevated, agitated, or irritable mood
- Rapid speech and racing thoughts
- Easily distracted
- Decreased sleep
- Impulsive, risk-taking behavior
What is hypomania?
Hypomania displays mood changes with behaviors that interfere with quality of life. A manic episode lasts for at least 7 days. A hypomanic episode lasts for 4–6 days.
Note: A hypomanic episode is less severe than a manic episode, with the later disrupting life activities.
Symptoms of depressive episodes
- Feelings of sadness and hopelessness, worthlessness and guilt
- Loss of interest in activities
- Weight changes
- Sleep problems (too much or too little sleep)
- Fatigue and lack of ability to focus
- Others noticing slowed behavior
- Potentially suicidal thoughts
How to diagnose bipolar disorder
Bipolar disorder is typically diagnosed during late adolescence (teen years) or early adulthood. Occasionally, bipolar symptoms can appear in children.
Diagnosing bipolar should always be done by a psychiatrist or qualified healthcare professional. It typically involves a multi-step process including interviews, mood charting, physical exam, lab tests, evaluations and observation. The diagnosis is made based on the DSM-5 criteria for the disorder.
Treatment for bipolar disorder
Bipolar disorder requires life-long management. Treatment goals are mood stabilization and improving functioning by reducing the severity and frequency of mood episodes.
Treatment options include:
- Pharmacological treatment with mood stabilizers, antipsychotics, antidepressants, or benzodiazepines for short-term intervention
- Psychotherapy, especially cognitive behavioral therapy
- Electroconvulsive therapy for severe cases
- Other measures like support groups, lifestyle and coping advice, and hospitalization when needed (e.g., risk of self-harm)
How often does ADHD co-occur with bipolar disorder?
When ADHD and bipolar co-occur, distinguishing between the symptoms can be challenging, since there can be overlap. Research indicates that there’s a higher prevalence of ADHD in individuals with bipolar disorder and vice versa, with some sources citing a co-occurrence rate of 20–30%. Both of these conditions need different therapeutic approaches, so clearly identifying and treating them is vital for positive outcomes.
Borderline personality disorder vs bipolar disorder
Borderline (BPD) is a personality disorder, while bipolar is a mood disorder.
Borderline is characterized by chronic patterns of unstable relationships, mood, and impulsivity with prominent fears of abandonment. Bipolar disorder is characterized by episodic/cyclical mood swings between mania/hypomania and depression.
Mood shifts are a symptom of both disorders, where they will be rapid and often triggered by interpersonal events in BPD, and not typically tied to any external events in bipolar disorder.
Treatment includes psychotherapy in both disorders, but medication is more prevalent in bipolar disorder.