What is ADHD?
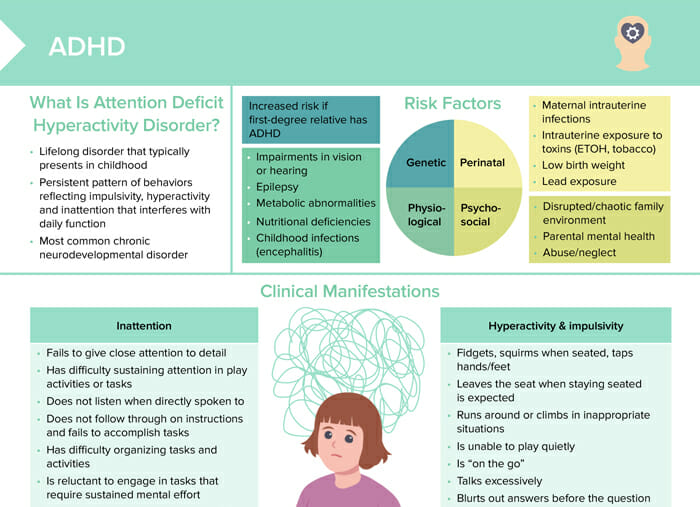
ADHD is the most common neurodevelopmental disorder. It is characterized by a persistent pattern of behaviors reflecting impulsivity, hyperactivity, and inattention that interferes with daily function. ADHD typically presents in childhood and is a lifelong disorder.
Related videos
Who is most likely to be diagnosed with ADHD?
Overall, state estimates for ADHD diagnoses in children between 3 and 17 years vary from 6% to 16%.
Boys are generally more likely to be diagnosed (13%) than girls (6%).
Non-Hispanic Black and White children are more often diagnosed with ADHD (12% and 10%, respectively) than Hispanic (8%) or Asian children (3%).
What is ADHD in adults?
ADHD in adults often manifests differently than in children. Adults may not exhibit overt hyperactivity as children often do. Instead, they may experience:
- Trouble focusing and being easily distracted
- Difficulty in organizing and completing tasks
- Being forgetful in daily activities
- Impulsiveness and impatience
- Poor time management
- Restlessness and difficulty relaxing
- Frequent mood swings
Who can diagnose ADHD?
ADHD is typically diagnosed by psychiatrists, psychologists, or neurologists who have undergone specialized training in diagnosing and treating mental health disorders. In some cases, primary care physicians who are well versed in adult ADHD may also make a diagnosis. The diagnostic process usually involves a thorough medical evaluation, mental health screening, and the use of ADHD-specific rating scales.
As a nurse, you can recognize ADHD in your clients by noticing the signs and symptoms, in addition to understanding their medical and psychiatric history, and refer your suspicions and concerns to the qualified responsible healthcare provider.
How to test for ADHD
Testing for ADHD often involves several steps:
- In-depth exams to rule out other causes for symptoms
- Client interview for symptoms, history, and functioning, as well as family, school, work, and medical history; also asking family
- ADHD rating scales (questionnaires) and other psychological testing
- Observing the client for behaviors in different settings
Remember, it’s critical to have these assessments conducted by a professional qualified in diagnosing ADHD.
What causes ADHD?
Risk factors associated with ADHD include:
- Genetic:
- Increased risk if ADHD present in a first-degree relative
- Physiological:
- Vision or hearing impairments
- Epilepsy
- Metabolic abnormalities
- Nutritional deficiencies
- Childhood infections
- Perinatal:
- Maternal intrauterine infections
- Intrauterine exposure to toxins
- Low birth weight
- Lead exposure
- Psychosocial:
- Disrupted or chaotic family environment
- Parental mental health problems
- Abuse/neglect
What are the ADHD types?
The three main subtypes are:
- Predominantly inattentive: difficulty paying attention, easily distracted, but not overly active (formerly known as ADD)
- Predominantly hyperactive-impulsive: restlessness and impulsivity (Hyperactivity tends to decrease with age, but impulsivity can continue into adulthood.)
- Combined: both inattentive and hyperactive-impulsive symptoms
ADHD symptoms
Clinical manifestations of ADHD can be categorized into signs of inattention and signs of hyperactivity and impulsivity.
Inattention
- Fails to give close attention to detail
- Has difficulty sustaining attention in play activities or tasks
- Does not listen when directly spoken to
- Does not follow through on instructions and fails to accomplish tasks
- Has difficulty organizing tasks and activities
- Is reluctant to engage in tasks that require sustained mental effort
- Loses things necessary to accomplish activities
- Is easily distracted by extraneous stimuli
- Is forgetful in matters of daily activities
Hyperactivity & impulsivity
- Fidgets, squirms when seated, taps hands/feet
- Leaves the seat when staying seated is expected
- Runs around or climbs in inappropriate situations
- Is unable to play quietly
- Is “on the go”
- Talks excessively
- Blurts out answers before the question is complete
- Has trouble waiting their turn
- May interrupt others
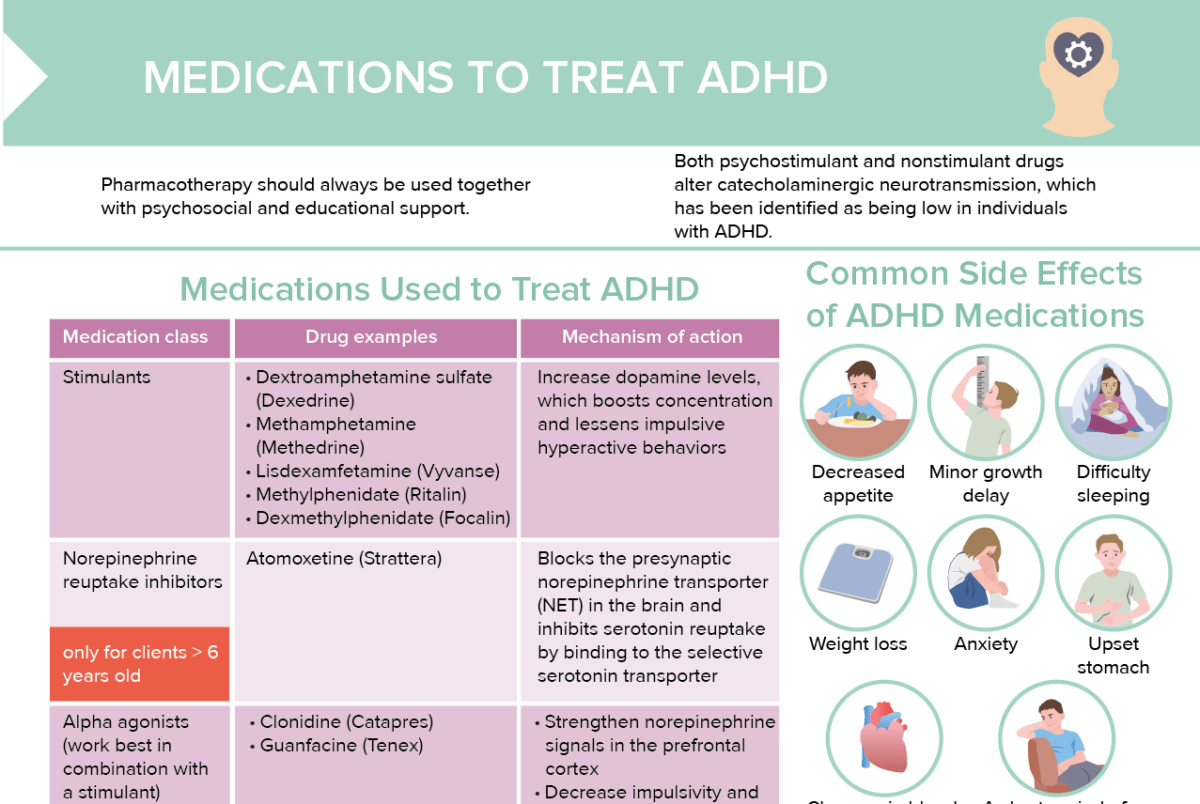
How is ADHD treated?
Non-pharmacologic treatments for ADHD include:
- Behavioral therapy
- Behavioral interventions in the classroom
- Organizational skills training
- Peer interventions that focus on behavior
- Educational support
- Support groups
Read more about ADHD medications here →
What is the difference between ADD and ADHD?
ADD (Attention Deficit Disorder) and ADHD (Attention-Deficit/Hyperactivity Disorder) are often used interchangeably, but there is a distinction.
Originally, ADD was used to describe people who have trouble focusing but do not display hyperactivity. On the other hand, ADHD was used to describe people who are hyperactive as well as inattentive.
However, since the 1994 edition of the DSM, all forms of the disorder, including those without hyperactivity, are officially known as “ADHD” with three subtypes: predominantly inattentive, predominantly hyperactive-impulsive, and combined.
So, in contemporary usage, ADD is generally considered an outdated term and is encompassed within the broader diagnosis of ADHD, predominantly inattentive type.
How often does ADHD co-occur with bipolar disorder?
ADHD and bipolar disorder can co-occur, but the exact prevalence can vary. Research has found that up to about 20% of people with bipolar disorder also have ADHD. Conversely, around 5–20% of those with ADHD also have bipolar disorder. These rates are significantly higher than in the general population.
Both conditions share some symptoms like impulsivity and mood instability, making the diagnostic process more complex. Any suspicion of co-occurrence should be evaluated by a qualified healthcare provider for proper diagnosis and treatment.