What is acute kidney injury?
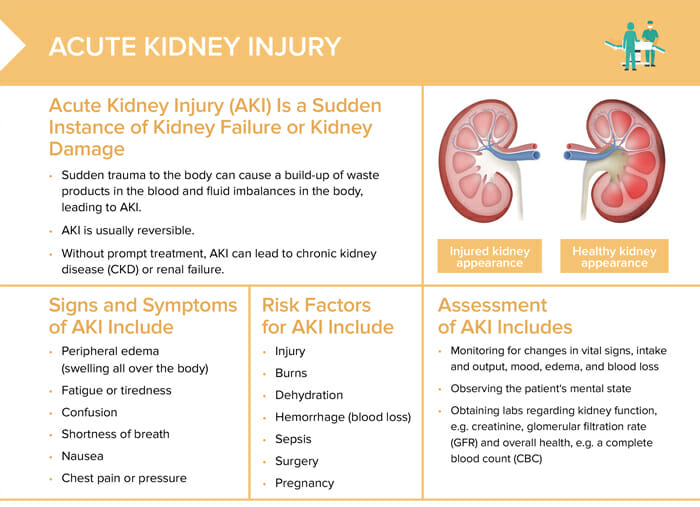
Acute kidney injury is a sudden instance of kidney failure or kidney damage. While being usually reversible, without prompt treatment, acute kidney damage can lead to chronic kidney disease or renal failure.
Criteria for acute kidney injury
- Rise in serum creatinine (> 0.3 mg/dL or > 50%)
- Reduction in urine output (< 0.5 mL/kg for > 6 hours)
Note: The expected range for creatinine is 0.7–1.4 mg/dL (62–124 mmol/L).
What is the most common cause of acute kidney injury?
One of the most common causes of acute kidney injury is decreased blood flow to the kidneys, for example due to dehydration, blood loss, burns, or sepsis.
Other causes include:
- Damage to the kidney tissue (e.g. acute tubular necrosis, glomerulonephritis, vasculitis, or acute intestinal nephritis)
- Obstruction of urine outflow (e.g. kidney stones or tumors)
Risk factors
- Injury
- Burns
- Dehydration
- Hemorrhage
- Sepsis
- Surgery
- Pregnancy
Symptoms and pathophysiology of acute kidney injury
Signs and symptoms of acute kidney injury
- Peripheral edema
- Fatigue
- Confusion
- Shortness of breath
- Nausea
- Chest pain or pressure
Pathophysiology
Pathophysiologic effects of acute kidney injury on electrolytes and acid-base balance:
- Hyperkalemia
- Hyperphosphatemia
- Metabolic acidosis
Nursing interventions for acute kidney injury
- Monitor for changes in vital signs, intake and output, mood, edema, and blood loss, overall health lab values (e.g. CBC)
- Observe client’s mental state
- Obtain labs regarding kidney function: creatinine, glomerular filtration rate
- Restore fluid balance
- Prevent infection
- Improve nutritional intake
Nursing diagnoses for acute kidney injury
- Acute pain: due to inflammation and increased pressure within renal capsule
- Excess fluid volume: monitor weight/output, assess for signs of fluid overload like edema; possible orders: diuretics, fluid restriction
- Impaired urinary elimination: monitor intake/output, electrolytes
- Risk for electrolyte imbalance: monitor serum electrolyte levels and assess for signs or electrolyte imbalances
- Knowledge deficit: provide education on disease, management, medications, dietary restrictions