What goes into managing pain after surgery?
Effective postoperative pain control facilitates early mobilization, reduces hospital length of stay and improves client satisfaction. Opioid medications remain central to pharmacologic postoperative pain management. However, given growing awareness of the morbidity and mortality associated with opioid use disorders, best practice increasingly supports a multimodal and multidisciplinary team approach.
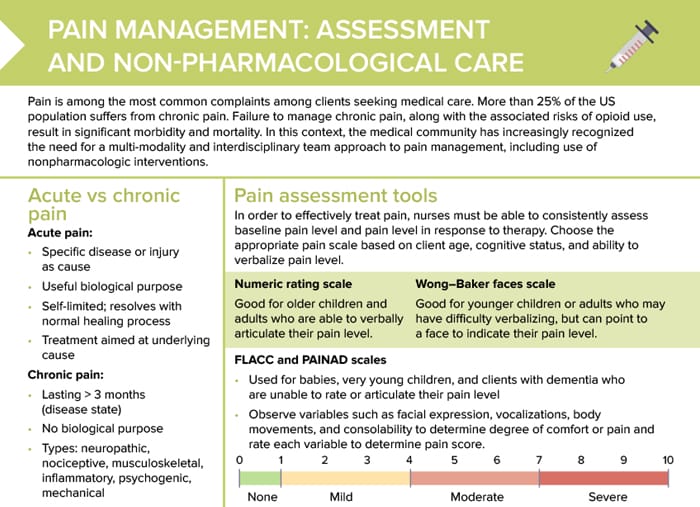
Preoperative planning
Planning for pain management should begin in the preoperative period. Factors to consider include:
- Type of procedure anticipated
- Client age
- Comorbidities
- History of chronic pain, depression, chronic opioid use
- Social factors
- Client openness to or current use of alternative and complementary therapies
Nursing considerations about pain management
- Pain scale indications should be included in each drug order for pain control. Select drugs based on the client’s reported pain level. Be sure to document pain level assessment to validate selection and timing of pain medications.
- Always adhere to ordered reassessment schedule to verify efficacy of pain control. Timelines differ based on the class, dose, and route of medication administered.
- Pain medication may be scheduled or ordered PRN (‘as needed’). Review orders and assess client pain frequently to ensure adequate pain control through use of PRN medications.
Patient-controlled anesthesia (PCA) pump
A PCA pump allows clients to self-manage pain by pressing a button for medication or administering a constant low dose with optional supplemental bolus doses initiated by the client. Nursing tasks:
- Assessment, pump maintenance, and client education
- Monitor carefully for signs of oversedation.
- Educate that the button may be pressed by the client only, not by family members or other visitors.
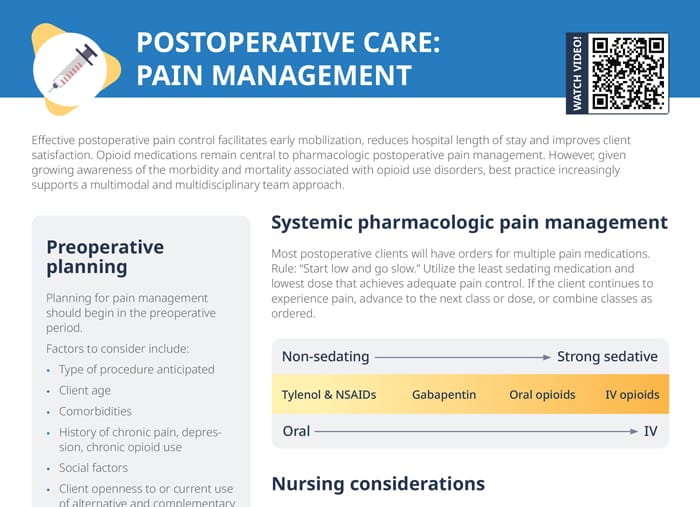
Systemic pharmacologic pain management
Most postoperative clients will have orders for multiple pain medications.
Rule: “Start low and go slow.”
Utilize the least sedating medication and lowest dose that achieves adequate pain control. If the client continues to experience pain, advance to the next class or dose, or combine classes as ordered.
Medications in order of least to most sedating:
- Tylenol and NSAIDs
- Gabapentin
- Oral opioids
- IV opioids
How to relieve pain after surgery naturally
Natural methods to relieve postoperative pain
When considering natural methods, it’s important to discuss them with the healthcare team to ensure they are safe and appropriate for the patient’s specific situation, especially in the postoperative context. These methods are often most effective when used as part of a comprehensive pain management plan that may also include medications.
- Physical therapy, movement, early ambulation
- Heat or cold therapy
- Rest and relaxation techniques
- Massage, acupressure (never on surgical wounds)
- Aromatherapy (mindful of allergies)
- Herbal supplements
Multimodal approach
Layered interventions, tailored to each client’s characteristics, comorbidities, and risk factors, improve pain management. Nurses can encourage the multidisciplinary team to plan for multiple modalities:
- Systemic pharmacologic therapy
- Local, intra-articular, or topical techniques
- Regional anesthetic techniques
- Neuraxial anesthetic techniques
- Nonpharmacologic therapies
How to get rid of gas pain after surgery
Post-surgical gas pain is common and uncomfortable for patients. Encourage your nursing clients to move and walk around as soon as their condition allows. Comfortable positioning and hydration, as well as warm compresses, deep breathing exercises, and dietary adjustments can help as well.
How to treat nerve pain after surgery
- Prescribed pain medications may include neuropathic pain agents like gabapentin or pregabalin: Monitor for effectiveness and side effects.
- Non-pharmacological interventions include physical therapy, heat and cold therapy, and relaxation techniques.