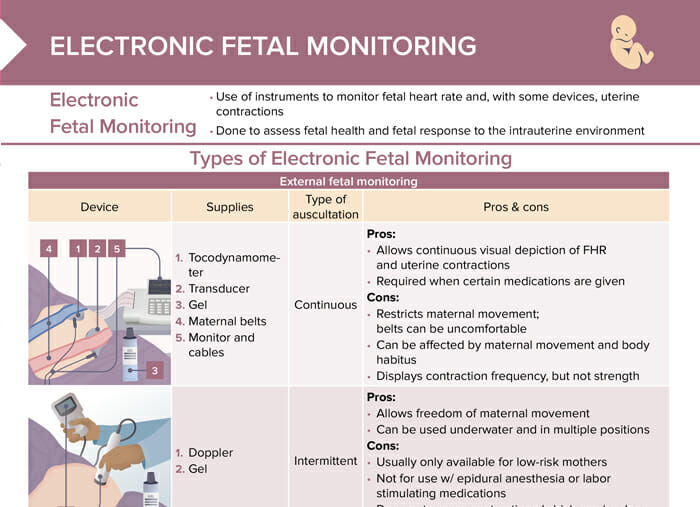
What is electronic fetal monitoring?
Electronic fetal monitoring is the use of instruments to monitor fetal heart rate and uterine contractions to assess fetal health and response to the intrauterine environment.
What are the types of electronic fetal monitoring?
The types of electronic fetal monitoring are:
- External fetal monitoring: uses a tocodynamometer and a transducer
- Internal fetal monitoring: uses a fetal scalp electrode and an intrauterine pressure catheter
What are the supplies needed for electronic fetal monitoring?
External monitoring:
- Continuous auscultation:
- Tocodynamometer
- Transducer
- Gel
- Maternal belts
- Monitor and cables
- Intermittent auscultation:
- Doppler
- Gel
Internal monitoring:
- Fetal scalp electrode
- Intrauterine pressure catheter
- Monitor and cables
- Sterile gloves, gel, syringe to flush, tape
What are the pros and cons of the types of fetal monitoring?
| Type of monitoring | Pros | Cons |
| External; continuous auscultation | Allows continuous visual depiction of fetal heart rate (FHR)and uterine contractions (required when certain medications are given) | Restricts maternal movement (belts can be uncomfortable); can be affected by movement and body habitus; displays contraction frequency but not strength |
| External; intermittent auscultation | Allows freedom of maternal movement and can be used underwater and in multiple positions | Usually only for low-risk mothers; not for use with epidurals or labor-stimulating medications; does not assess contractions |
| Internal (continuous auscultation) | Most accurate! Provides continuous visual depiction of FHR and uterine contractions; only method that can objectively assess contraction strength; unaffected by maternal habitus/movement; can be used to provide amnioinfusion | Placed by provider; requires cervix to be dilated and ruptured membranes; increases risk of infection; possibility of injury; contraindicated with some maternal conditions/infections; restricts maternal movements |
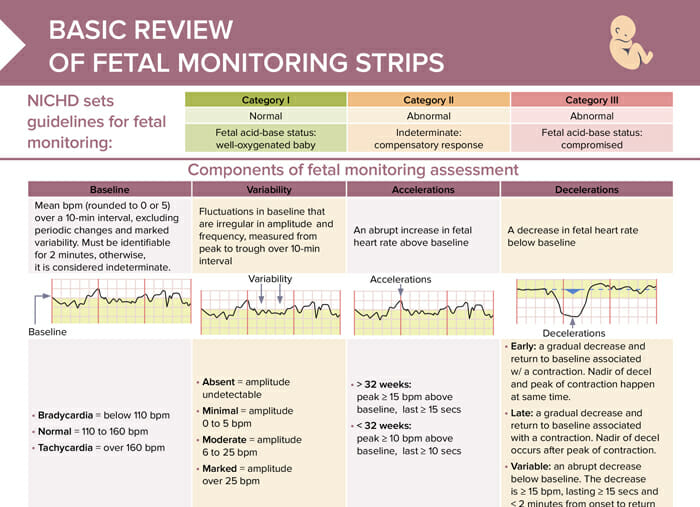
What are the components of fetal monitoring assessment?
The components of fetal monitoring assessment include:
- Baseline: mean bpm (rounded to 0 or 5) over a 10-min interval, excluding periodic changes and marked variability; must be identifiable for 2 minutes, otherwise considered indeterminate
- Variability: fluctuations in baseline that are irregular in amplitude and frequency, measured from peak to trough over 10-min interval
- Accelerations: abrupt increase in FHR above baseline
- Decelerations: decrease in FHR below baseline
NICHD guidelines for fetal monitoring
The National Institute of Child Health and Human Development (NICHD) has developed a three-tiered system for the interpretation of FHR patterns through electronic fetal monitoring:
| Category I | Category II | Category III |
| Normal | Abnormal | Abnormal |
| Fetal acid-base status: well-oxygenated baby | Indeterminate: compensatory response | Fetal acid-base status: compromised |
How to interpret values of fetal heart rate monitoring
Baseline
The baseline fetal heart rate is the average FHR during a 10-minute window, excluding periods of marked variability, decelerations, and tachycardia.
- < 110 bpm = bradycardia, may be due to fetal hypoxia
- 110–160 bpm = normal
- > 160 bpm = tachycardia, potentially from maternal fever or fetal distress
Variability
Variability refers to the fluctuations in the baseline FHR. Moderate variability (6 to 25 beats per minute) is usually a reassuring sign, indicating a well-oxygenated fetus with a functioning autonomic nervous system. Minimal or absent variability can be concerning and may suggest hypoxia or acidemia, but can also be seen in a sleeping fetus or with certain medications.
- Absent: amplitude undetectable
- Minimal: amplitude 0–5 bpm
- Moderate: amplitude 6–25 bpm
- Marked: amplitude > 25 bpm
Accelerations
Accelerations are temporary increases in the FHR of at least 15 beats per minute, lasting for at least 15 seconds. They’re generally a reassuring sign, indicating a well-oxygenated fetus responding to movement or stimulation.
- > 32 weeks: peak ≥ 15 bpm above baseline, last ≥ 15 secs
- < 32 weeks: peak ≥ 10 bpm above baseline, last ≥ 10 sec
Decelerations
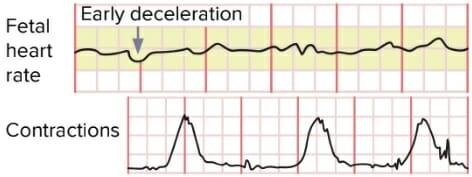
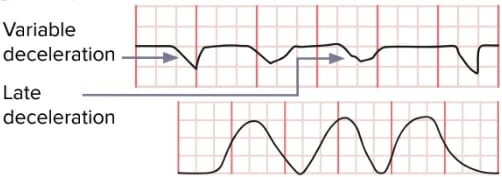
Early decelerations are dips in FHR that coincide with contractions, usually due to head compression and are generally not concerning. Late decelerations are dips in FHR that occur after the peak of a contraction and may indicate placental insufficiency, necessitating close monitoring or intervention. Variable decelerations are abrupt drops in FHR due to umbilical cord compression. Depending on their frequency, depth, and duration, they may require intervention.
- Early: a gradual decrease and return to baseline associated w/ a contraction. Nadir of decel and peak of contraction happen at the same time.
- Late: a gradual decrease and return to baseline associated with a contraction. Nadir of decel occurs after the peak of contraction.
- Variable: an abrupt decrease below baseline. The decrease is ≥ 15 bpm, lasting ≥ 15 secs and < 2 minutes from onset to return to baseline.
Bonus download
Review of fetal monitoring strips
Overview of fetal monitoring strip assessment, review of category 1–3 strips, and basic interventions
Nursing tips for fetal monitoring assessment
Variable and late decelerations require immediate intervention:
- Reposition
- Oxygen 10 L/min
- Cervical exam
- Turn off oxytocin.
- Fluid bolus
- Call provider.
The first nursing intervention for an abnormal fetal heart tracing is to reposition the client to their left side to maximize blood flow and oxygen to the fetus.
Fetal monitoring strip examples
Normal fetal heart rate tracing (NICHD category I)
- Baseline: 110–160 bpm
- Variability: moderate
- Accelerations: present
- Decelerations: none or early decelerations only
Abnormal fetal heart rate tracing (NICHD category II or III)
- Baseline: < 110 or > 160 bpm
- Variability: absent, minimal, or marked
- Accelerations: none or less than expected for gestational age
- Decelerations: variable, late decelerations present