Introduction
Given its ubiquitous nature, learning feels like a natural part of our day-to-day life, mentioned as frequently in academia as it is in daily conversation, often without recognizing the depth and breadth of its history. It has evolved inexorably from philosophical discussions to become an entire scientific discipline. Multiple great thinkers and researchers have postulated various learning theories that have informed and allowed future researchers to build upon them, creating modern theories. As years passed, conceptual research on what learning is and how it happens shifted over to experiments that attempted to delineate how people learn best and how to scale it up to improve education. Eventually, this made its way to medical education, which enabled the investigation and application of empirically supported techniques. This allowed both teachers and students to differentiate which techniques are effective and which ones are not. Given this progress and the increasingly widespread availability of evidence-based medical education resources, it has become more important than ever for educators and students to access and integrate these methods into their teaching and learning.
History of Learning as a Concept
The discussion surrounding learning started millennia before the modern day, dating back to Ancient Greece and the minds of philosophers such as Plato and Aristotle.(1) Before learning was phrased as theories, it originated from philosophical positions on what knowledge is and how it came to be in human beings (i.e., how humans “learn”). During this phase, it was divided into two general positions: rationalism and empiricism.(1)
Rationalism came first, whereby it was believed that knowledge comes ultimately from reason, is innate, and may happen even without external stimuli. Plato, René Descartes, and Immanuel Kant are prominent contributors to this position. Plato believed that knowledge can come purely from innate reasoning, whereas Descartes and Kant considered that it is affected in some manner by experience gained and external stimuli, respectively.(1)
In contrast, empiricism believes knowledge to come solely from experience, to not be innate, and to not exist independent of external experience. Aristotle, John Locke, George Berkeley, David Hume, and John Stuart Mill are all well-known subscribers to this belief. As a subset of empiricism, Aristotle believed that association between objects strengthens memory (associative learning). Locke and Mill, while differing in some core assumptions, are notable associationists, alongside Aristotle.(1)
Interestingly, these schools of thought also appear in medicine. There were groups subscribing to beliefs of the same name that differentiated their approach toward illnesses and their treatment. Rationalism in medicine was championed by Hippocrates and his sons, and focused more on rationalizing the source of the disease, or in other words, the how of it. In modern vernacular, this translates as being focused on the pathophysiology of an illness, believing that “where observation failed, reason might surprise.”(2) Empiricism, however, disagrees, preferring to focus on the what of a disease, i.e., the symptoms, remedies, similarities, and outcomes of illnesses, building upon past experiences to deduce the optimal treatment in order to produce the best outcome.(2)
Learning theories were approached in a more scientific manner with the advent of systematic research into psychology in the early 19th century, with psychologists such as Wilhelm Wundt and Hermann Ebbinghaus paving the way. Wundt founded the first Department of Psychology in 1875 in Leipzig, Germany, where he conducted experiments and founded a journal on psychological research.(1,3) Around the same time, Ebbinghaus, a prolific researcher in his own right, pioneered seminal research on memory, which produced the Forgetting Curve.(1,4) His research findings have subsequently been validated by replications of the curve in modern papers (see Murre and Dros, 2015).(4) Afterwards, precursors to modern learning theories continued to be developed by different scientists, such as Edward Titchener, who developed structuralism, as well as John Dewey and James Angell, who were prominent functionalists.(1,3) These theories eventually led to the popularity of behaviorism, pioneered and popularized by Edward Thorndike, Ivan Pavlov, and Burrhus Frederic Skinner, which led to its status as one of the most commonly held learning theories from the 1950s onward.(1,5) All of these theories continuously informed, dissented, and eventually grew into the theories of learning to which we subscribe today.
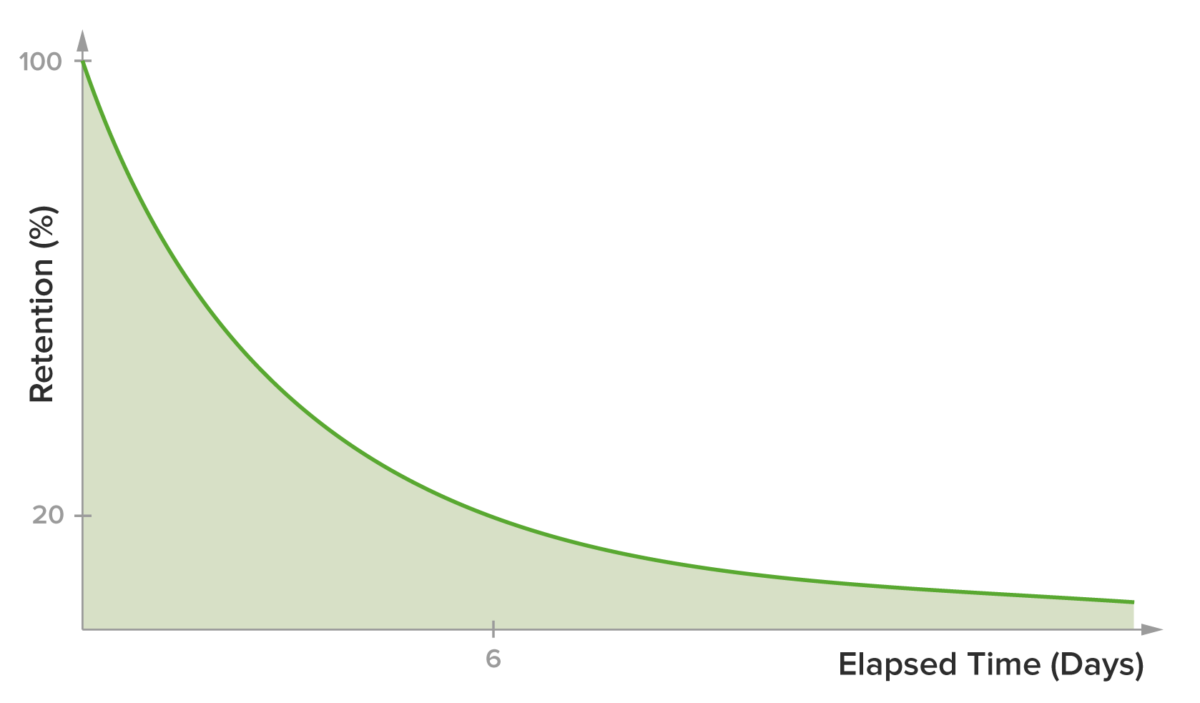
Figure 1. Typical Representation of the Ebbinghaus Forgetting Curve
Learning Science and Learning Theories
Learning theories are theories that put forward hypotheses describing how learning happens.(6) Over the years, many theories have been developed to achieve this purpose. However, none of them were able to fully illustrate the breadth of the learning process on their own.(7) Richard E. Mayer made an important point that highlights the relationship between learning theories and research evidence. In his book on multimedia learning, he claims that research evidence forms the basis of the theories. These theories, in turn, inform research and provide a hypothesis as a base for their investigation.(8) Many researchers have argued that a working understanding of learning theories would help educators teach better by allowing them to 1) combine elements of different theories and better implement them in different situations(9), 2) set better learning objectives, choose more appropriate instructional strategies, and implement better evaluation strategies(10), and 3) understand that individual differences apply and that the responsibility for student performance should be attributed to these differences as well.(5)
A notable concept that had a lot of influence in the development of teaching strategies for adults is “andragogy.” Coined by Alexander Kapp in 1833 and popularized by Malcolm Knowles in 1988, this term differentiates learning in adults from learning in children, postulating that adults have different motivations and needs to learn, as well as different kinds of experience prior to learning.(5,7) Despite being seen by some as an unnecessary distinction, many researchers still support this theory, as it helps not only in tackling the differences between professional knowledge gained from an adult’s learning activities and prior knowledge, but also in analyzing how an adult’s versus a child’s behavior and mindset affect their learning.(5)
The following is an overview of notable learning theories relevant to medical education. It is based on several publications that phrase the theories specifically toward their application in medicine.(5,7,10)
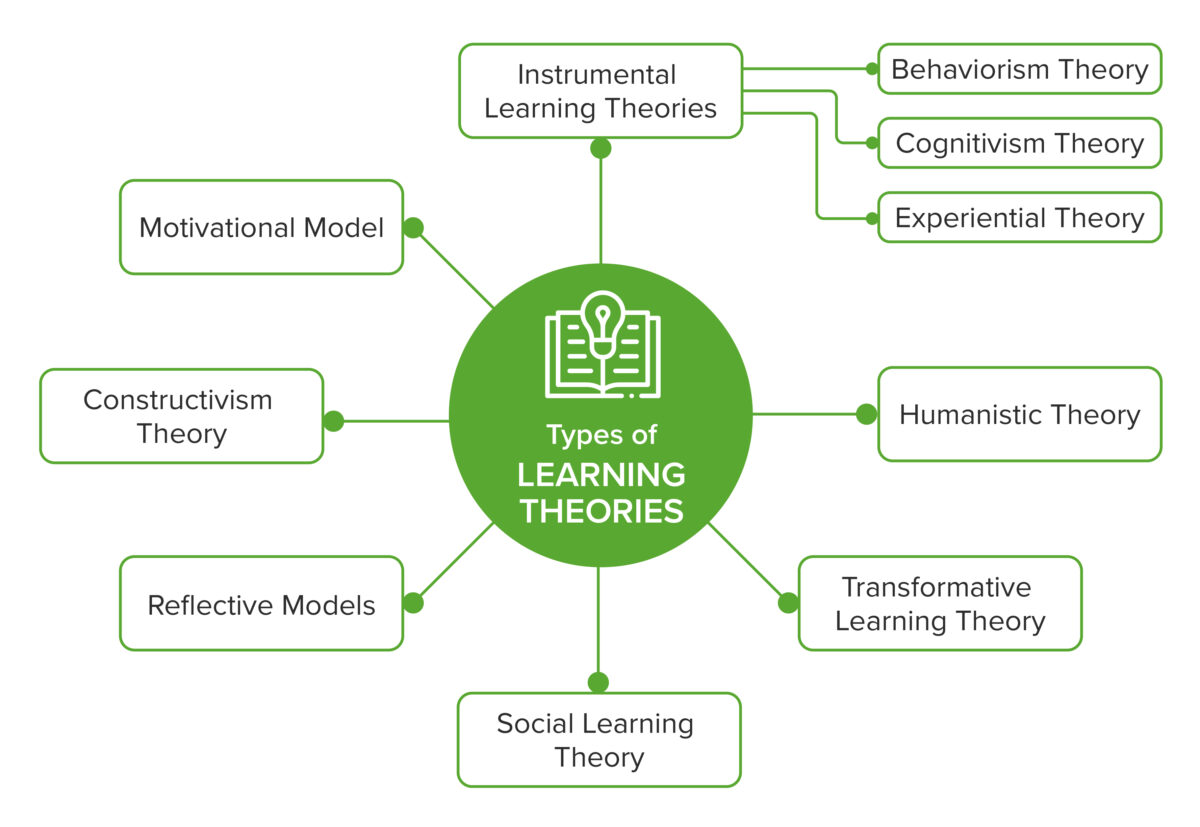
Figure 2. Overview of the learning theories in the context of medical education
Instrumental Learning Theories focus on the experience of individuals, their relationship with the experience they gained, and stimuli from external environments(5,7). These include the following three theories:
- Behaviorism: This is a theory in which learning is defined as a change in behavior that occurs as a result of a stimulus from the learner’s external environment.(5,7,10) Its principle is rooted in the understanding that learning comes from observing behavior and that mastering prior steps before moving to subsequent ones is indispensable.(10) This learning theory lends itself more to a teacher-centric style. The educator is required to control the learning environment to produce the desired result. In this case, positive reinforcement promotes a behavioral change, while negative consequences weaken it.(5) In medical education, the use of behaviorism helps in creating competency-oriented teaching and assessment strategies, which include “clinical skills instruction and simulated case scenarios.”(10) This is to say that, in knowing the target behavior and recalling the principles of behaviorism, teachers will be able to better set and communicate learning objectives to students. Consequently, students will better understand what behavior is expected of them, how it should be performed, and what defines success in their performance.(10)
- Cognitivism: Almost opposite to behaviorism, this is a theory in which learning is essentially said to come from within, the locus of it being the internal environment and cognitive structures of the learner.(10) As opposed to a behaviorist approach, a cognitivist approach concerns itself more with information processing, internal reflections, and the student’s process of breaking down concepts that are being learned to understand their roots.(7,10) In this case, the teacher’s role is to facilitate “learning how to learn” in students. In medical education, it is most applicable in the construction of concept maps and the facilitation of reflective thinking in students by their teachers, which medical educators can do by asking the student to recall and reflect on what they learned from a case they encountered during their ward rounds. (10)
- Experiential: This theory proposes that learning happens through experiencing the material or, in other words, through the “interaction with the authentic environment.”(5) Thus, the teacher would have the obligation to design, prepare, and provide the appropriate environment for the students to be exposed to the desired knowledge source. In medicine, this is usually relevant in clinical teaching, where educators aim to develop specific skills and behavior to fit real-life situations by adding teaching components that expose students to real or simulated versions of those situations.(7)
Humanistic Theory places a much greater emphasis on self-directed learning and is deeply related to “andragogy.” It suggests that adults have the autonomous capability to plan, direct, and evaluate their own learning, which is related to the need of individuals to achieve their full potential (self-actualization). In this theory, the onus of learning is placed on the students, with teachers as facilitators of learning.(5,7,10) While critics question the effectiveness of fully autonomous learning as opposed to directed self-learning(7), the theory remains important to consider. As the advent of technology makes a quality application of this theory easier than ever, focusing on humanistic principles will support us in putting autonomous and self-directed learning at the forefront of our educational strategies, through the use of simulations, role-play, and self-assessments.(10) In applying this theory, teachers will also know to support learning in students through “facilitative learning”, instead of didactic teaching, which is particularly useful to foster clinical reasoning in tackling difficult cases.(5)
Transformative Learning Theory utilizes critical reflection to challenge the learner’s prior beliefs, which subsequently creates a change in meaning or context to those perspectives.(5,7) In this theory, learning happens when the learner finds a problem and understands that it is different from past perspectives. This is followed by the learner’s critical reflection, which engages metacognitive thinking on their part, and is followed by an action taken by the learner based on this reflection, which results in a change of perspective (learning).(5) Transformative Learning Theory is used in medical education through group discussions or analytic learning activities, in which the medical educator motivates and facilitates the learning process via case studies, and learners then reflect on past assumptions and share ideas with their peers.(5,11)
Reflective Models are learning theories that put reflection by the learner at the center of how learning happens. They believe that learning happens when students reflect on the experiences they gained in practice and create action to produce a change in the meaning of these experiences for themselves. It differs from transformative learning in the degree of reflection that it entails: transformative learning involves critical reflection, which requires a higher order of thinking than simple reflection.(5) Schön (1987) divides reflection into two types: on learning and in learning, with the former happening after the action and the latter occurring during the action itself.(12) In medical education, reflection on learning allows students to build learning systems for themselves and foster a habit for reflection in their practice, whereas reflection in learning acts as an important instructional tool that educators can use to improve competence in students by facilitating reflection on their experiences.(5) Ultimately, this model adopts reflection and feedback as an important competency building tool and permits educators to gain insight into their students’ learning and thinking processes for further self-directed learning.(7)
Social Learning Theory combines behavior modeling with cognitive learning. It hypothesizes that learning happens through interacting with and observing the behavior of others (in a social context), but goes one step further than behavioral learning by subscribing to cognitive learning as well, i.e., that learning may happen through observation alone.(5,10) In this theory, the teacher demonstrates the behavior, guides the learners in implementing it, and provides opportunities for the learners to practice the behavior. It stands to reason that in medical education, Social Learning Theory is applicable in the concepts of mentoring, collaborative learning, and in teaching activities that involve case studies.(10) As an example, when applied in the settings of a mentor-mentee relationship and/or bedside teaching, the learners observe the behavior modeled by their teachers, they remember and understand the behavior being shown, they apply the behavior, and receive feedback on it for further learning.(5,10)
Motivational Model is a theory that incorporates two important factors into adult learning: motivation and reflection. The Motivational Model includes three significant theoretical models: Self-Determination Theory, Expectancy Valence Theory, and the Chain of Response Model.(5,7) The Self-Determination Theory stipulates that learning in adults is greatly affected by intrinsic motivation, which is determined by the need for autonomy, competence, and a feeling of belonging.(7) The Expectancy Valence Theory states that motivation to learn is affected by the learner’s expectancy of success, coupled with the value of this success.(5,7) The Chain of Response Model states that adult participation in learning is affected by internal motivating factors, including self evaluation, the attitude of the learner toward education, and the importance of goals and motivation.(5,7) While it is not taken into primary consideration when designing curriculum or teaching approaches, the Motivational Model is important to take into account when deciding on teaching strategies because, to a degree, student motivation is a natural outcome of good teaching strategies.(5)
Constructivism Theory is a relatively new theory that places emphasis on the compounding nature of learning and the cognitive mechanisms that learners engage in order to critically reflect on past knowledge.(5) This theory states that new knowledge is created by building on past skills and experiences with new ones that are gained through social activities. The meaning emerges from the learner’s reflection of the new experiences against the old ones.(5,10) In this theory, knowledge is relative, as it is always compared to and built from the experiences and environments of each individual learner. The role of educators, in this case, is to motivate learners to critically reflect on their knowledge and to negotiate the meaning of each new piece of knowledge with the learner, guiding them to the best possible answer.(10) In medical education, applications of this theory include group learning activities, the creation of course portfolios, practice narratives for students (reflecting on what they have learned from a case they encountered during their rotations), journal clubs, and critical appraisals.(5,10)
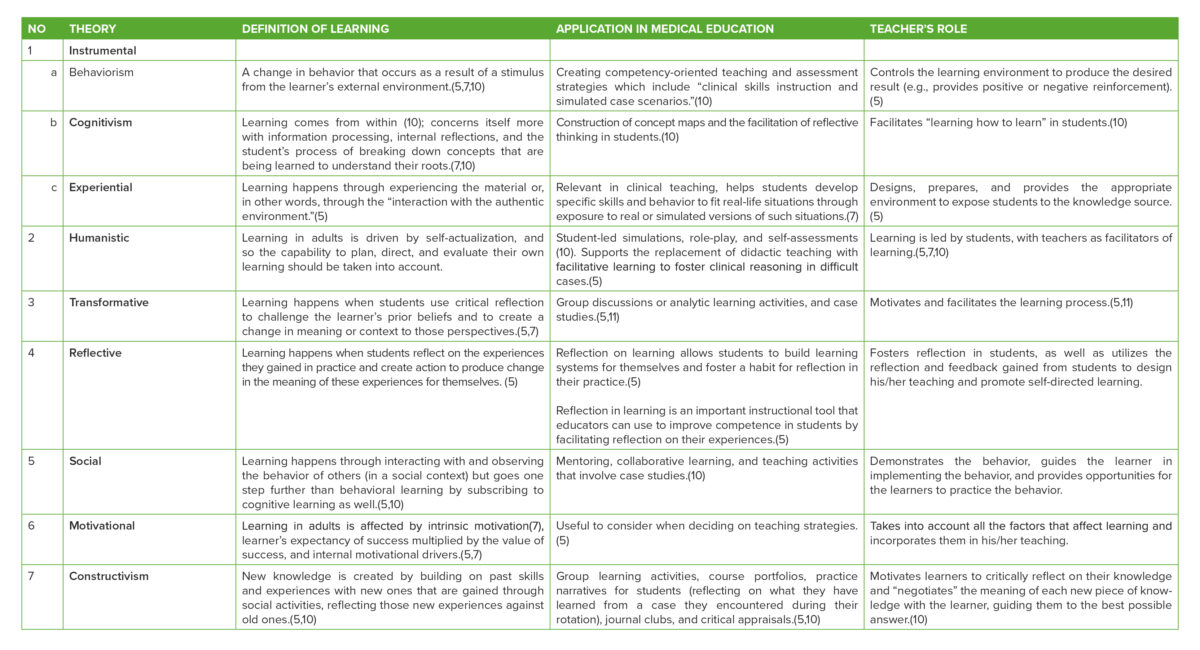
Table 1. Summary of learning theories, their medical education application, and teacher’s role (5–11)
Ineffective Learning Methods
A problem currently faced in medical education is that effective, theory-driven, and evidence-based techniques are being underutilized by both teachers and learners, while popular techniques that have been proven ineffective are more commonly adopted.(13) When we think of medical education, we often think of “traditional” teaching methods, such as large-group passive lectures and ineffective study methods such as rereading and cramming. These modalities, while showing benefit in certain situations, have been proven suboptimal techniques based on the available evidence (e.g., passive vs active lecture (14,15), massed vs spaced learning (16), re-studying vs spaced retrieval (13,17)). Possible reasons for this disconnect include the overwhelming number of techniques available to use or the lack of the subject’s exposure to these effective techniques, which lead to the aforementioned problems.(13) Oftentimes, students already understand which techniques are effective and which are not, but are unable to translate this understanding into real-world practice due to habitual cramming before exams.(18)
During their research for Make it Stick (19), the authors interviewed a medical student who changed his study approach based on learning science principles. Among the valuable insights he provided was the idea that some of these evidence-based strategies are not intuitive for students, and their implementation could “slow down” students’ learning processes. However, he experienced better and consistent results and recommends that students need to learn to “trust the process.”(19) The transformation that this student underwent – from convention to evidence – is a transformation that is needed on a systemic level in medical education. The following section details several suboptimal methods in learning, which are still widely used, and what available evidence says about them.
Traditional Lectures: Having large group lectures is a method that has dominated medical education, and education in general, for centuries.(20) It has lasted this long due to several factors, including that it is far more cost-effective when compared to small-group or problem-based lectures, which require more faculty members and space to implement.(15) Furthermore, traditional lectures also have proven effectiveness in conveying large amounts of information to many people at once, as well as usefulness in providing explanations in medicine.(21,22) However, an increasing number of research papers have shown that adding an active learning component to traditional lectures, or replacing them with active learning modalities, provides benefits to students. These benefits include ease in paying attention to the material, increased participation opportunities in learning, higher pass rates, and higher overall scores on examinations.(20,21)
A meta-analysis by Freeman et al. (2014) reviewed more than 225 studies that compared outcomes from traditional lectures versus active learning and found that students who participated in active learning received results that were 6% better than their traditional lecture counterparts. These students were also 1.5 times less likely to fail.(20) While there is concern that teachers used to the older method of didactic lecturing may be change-averse, an international multi-center study by Dash et al. (2020) found that the delegator teaching style (i.e., one that promotes collaboration among students and peer learning) was preferred in the evaluated cohort.(23) The challenge now is to bridge this gap and facilitate the process of shifting away from purely didactic lectures, which would most likely require collaboration at an institutional level.
Learning Styles: Another common misconception popular among students and teachers is that different students will learn better by using a particular learning style. This convention suggests that a student would learn better under certain conditions, using certain types of materials/instruction style, and/or utilizing certain types of “mental activity” (involving different levels of cognition).(24) It is hugely popular and has created an industry dedicated to producing even more “learning style determination” tests and guides. Some examples of “learning style models” include the “VARK” model (visual, auditory, read/write, kinesthetic), which divides styles based on the type of material that the learner is exposed to, and the Gregorc learning style model (abstract sequential, abstract random, concrete sequential, and concrete random), which divides styles based on the sequence and type of material presented.(25)
Several problems have been reported related to this particular convention: One such problem, mentioned by Coffield et al. (26), is that providing tests to label and/or labeling a student with a particular learning style may be limiting their potential instead, causing the student to avoid and eventually fail to learn important concepts that are not suited to their preferred style.(27) Another problem, mentioned in an embattled meta-analysis by Kavale and Forness, found that, once they had adjusted for methodology, tailoring instruction to a student’s preferred style did not yield a positive modality effect.(28) Additionally, a review by Pashler et al. in 2009, which attempted to find studies that empirically supported this convention, concluded instead that there is an insufficient amount of methodologically sound experimental research proving the validity of learning styles. Ultimately, the paper recommends educators explore many other evidence-based educational practices,(24) which includes strategies that will be discussed in subsequent articles, such as spaced retrieval, spaced learning, interleaving, dual coding, and retrieval-based strategies.
Despite this conclusion, it is still important to note that learning styles are not without their own merit; some researchers actually support the use of an adjusted version of the concept, believing instead that instruction modality should be adapted to fit the content as opposed to the learner’s preferred styles.(29) Hence, in choosing which recommendation to follow, teachers should apply the concept of Best-Evidence Medical Education (BEME) and scientifically assess which approach to take with regard to the convention of learning styles.
Highlighting Passages: Many students believe highlighting or marking important passages to be an easy, low-effort, go-to studying technique that helps them learn better.(13,30) In his paper, Dunlosky cited Idstein and Jenkins, who said that some students mark very little, while others mark almost all the text, especially when the text is saturated with factual content.(13,31) Theoretically, the technique works due to a phenomenon called the “isolation effect,” which causes distinctly different, or differentiated, ideas to appear prominently in a person’s memory, allowing them to recall an idea better when evaluated at a later time.(13) Research initially found that highlighting does not produce a superior result over simple reading.(31,32) However, when specific nuances in the research were considered, it showed that performance on questions pertaining to highlighted text was actually better and that a better outcome resulted when students actively highlighted text (i.e., they consciously thought about and chose what to highlight), as is evident in a review by Dunlosky et al.(13)
Additionally, Lorch, Lorch, and Klusewitz in Dunlosky stated that overmarking can be detrimental to the studying process due to the reduction in distinction from other parts of the passage and to the lower level of cognitive processing required to highlight a larger number of text passages.(13) When taking these two things into account, it is thus appropriate to conclude that highlighting passages can still be an effective technique, as long as the student uses it appropriately and only highlights objectively important parts of the passage, something that can be strengthened with training and guidance.(13)
Massed Practice can be considered the opposite of distributed (or spaced) practice, which will henceforth be referred to as spaced practice in this article. Massed practice is a very popular, though ineffective, technique that students often use to prepare for exams, in which they concentrate their learning in very short time spans with very little to no space between each study session.(13,16) Commonly known as cramming, the widespread use of this technique is most likely due to the metacognitive bias that the technique produces. Students feel that they have greater mastery over the material prior to the exam, and are able to score marginally better in a shorter interval, as visible in this experiment with math problems by Rohrer and Taylor in 2006.(33) Students may also prefer massed practice due to the feeling that it takes less time to study, thus leaving more time to perform other tasks(16), or due to the erroneous initial belief that cramming is as effective as the more time-consuming spaced learning.(13)
This was demonstrated in an experiment by Bahrick in 1979, cited by Dunlosky et al.(13) which showed that zero or shorter inter-study intervals (1 day) produce equivalent results in the beginning, but are vastly outperformed by longer intervals (30 days) in terms of long-term retention. This shows that evidence-wise, while cramming does have benefits, it only works in the short term, and is vastly outweighed in the long term by the benefits of spaced practice.(34) This statement is also applicable in the context of medical education, as we can see in an experiment by Breckwoldt et al.(16) which shows superior key-feature test performance in a group of students following a spaced version of an emergency medicine course when compared to a massed-version group. Furthermore, a study by Kommu et al.(35) also showed significantly better performance in a group of pediatric department students after they began practicing spaced learning.
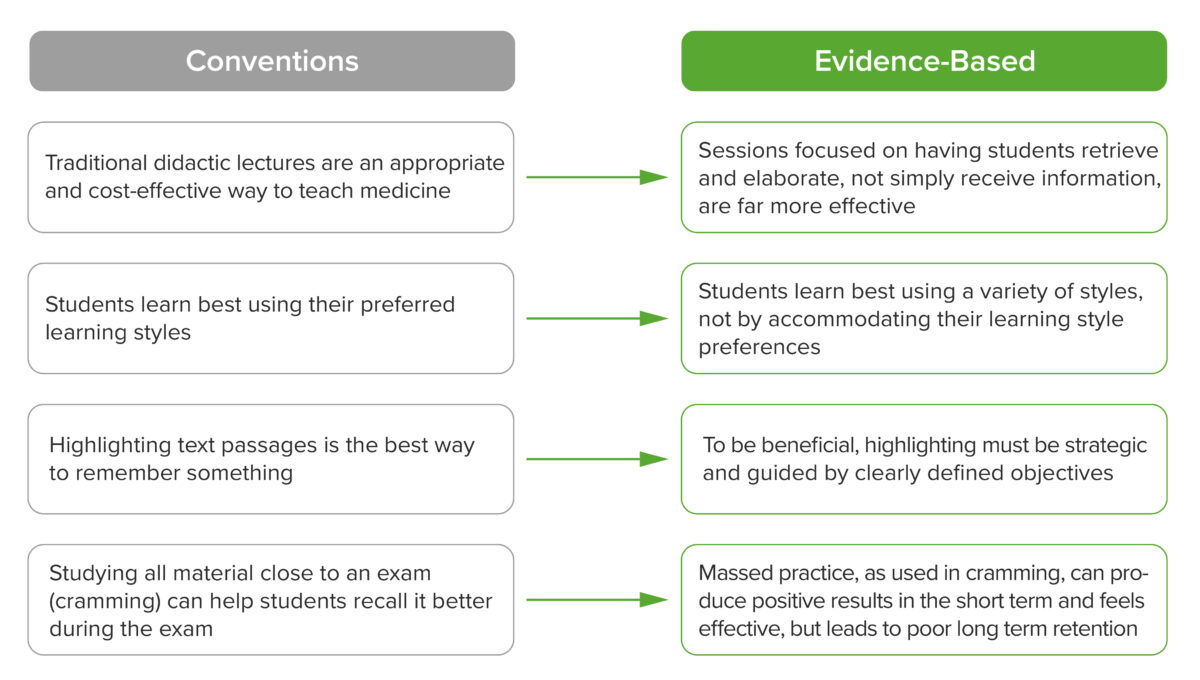
Figure 3. Ineffective conventions in learning vs. evidence-based learning principles
Evidence-Based Medical Education
The reason why we are able to know which techniques are useful and which ones are not is the advent and popularization of experiment-based classroom studies that evaluated the effectiveness of these strategies in real-life situations. These studies provide empirical evidence that allows educators and students to choose effective teaching and study techniques in an evidence-based manner in order to foster effective and durable learning in medical students and practitioners. Originally focused on the general field of education, Evidence-Based Education eventually became a topic of study within the field of medical education as well in the beginning of the 1950s.(36)
A historical review by Kuper, Albert, and Hodges (2010) pinpointed the year 1950 as the beginning of this shift, and the year 1959 as the more widespread institutionalization of medical education research (MER). This was driven mainly by socio-historical factors, such as(36):
- the increased importance placed upon scientific research beginning from the 1950s onward;
- improved funding availability for medical education research, whereby various grants began to support endeavors in MER (e.g., the Kellogg Foundation and the Commonwealth Fund);
- policy changes in accreditation that allowed for a more flexible approach to curriculum and education design in medicine;
- the need to keep up with exponential growth in medical knowledge, which was not balanced with a proportional increase in education length;
- concerns over and a renewed focus on accountability in the training of doctors from regulatory bodies and the general public; and
- other factors, such as the need to license foreign physicians following their influx post-World War II and a change to the American healthcare system that altered how training and treatments are performed.
This eventually drove educators to apply BEME, which is the act of applying an evidence-based lens to medical education. BEME is a term that featured prominently in the BEME Guide No. 1 by Harding et al., which made the case for a shift away from opinion-based teaching to an evidence-based approach in medical education, and provided several guiding steps on how educators can make this happen.(37,38) Reminiscent of the scientific process in evidence-based medicine, the five steps of BEME encourage educators and institutions to:
- Frame the (research) question the way one would frame a scientific question. Rather than using the PICO Model (Population, Intervention, Comparison, and Outcome), Masoomi cited Hammick in putting forward Participants, Educational Aspects, and Outcomes as the framing model for medical education.(38)
- Design a search strategy of common bibliographic databases, so the most appropriate research articles and evidence can be found.
- Use the QUESTS criteria, as suggested by Haig and Dozier(39), to evaluate the quality and usefulness of the evidence being investigated for use in a class. QUESTS stands for Quality (type of evidence and strength of the studies), Utility (how useful the evidence is and how it can be adjusted to fit the context in question), Extent (the amount of studies and their scope), Strength (how sure the conclusions in those research articles are), Target (how similar the expectations in the paper are when compared with the teacher’s), and Setting (how similar the setting of the research is with the teacher’s situation).
- Implement the change by applying the evidence found in a classroom setting, specifically when designing teaching strategies.(40)
- Evaluate the outcomes of the change(40) in order to make sure that educators are able to make an objective decision on the final adoption of the technique. Additionally, publication is recommended so outcomes can be referenced by other educators in the field.

Figure 4. BEME process (37,38)
Another notable milestone is the step forward in the combination of cognitive psychology and education. A grant was awarded to Henry L. Roediger III, Mark A. McDaniel, and nine other co-investigators by the James S. McDonnell Foundation in 2002 (19) which kick-started a ten-year collaboration between them that produced numerous research articles that helped “translate cognitive science into educational science.” While this research was not performed specifically in the context of medical education, it informed and galvanized research on the topic within the medical education community, as is evident by the numerous research projects in the past decade and their application in medical education.
Conclusion
Learning has a long and storied journey. It began as a philosophical topic and eventually became a focus of the scientific field of psychology(1,3). In medicine, it has also evolved from an opinion-based approach into an evidence-based one.(37,38) When we consider the importance o