Simplify Teaching and Assessing Clinical Reasoning
An innovative approach that demystifies clinical reasoning
The clinical reasoning process using Healer
Clinical reasoning is a multi-step, iterative process, often opaque and difficult to convey
Healer offers a new way to explicitly teach and assess these cognitive steps. It makes clinical reasoning easier for educators to teach and for learners to master, helping to improve patient diagnosis, management, and outcomes.
Healer demystifies clinical reasoning for learners and educators alike by breaking down the key elements of this complex process into discrete, but related skills of data acquisition, problem representation, hypothesis generation, and differential diagnosis. Healer offers a granular approach to practicing these skills while journeying through the stages of a clinical encounter, allowing learners to understand the reasoning process at a deep level while also yielding detailed and meaningful feedback for the learner and assessment insights for educators.
Through deliberate practice involving many clinical scenarios and disease processes, learners can use Healer to increase their self-awareness and their confidence, build and refine their clinical knowledge, and learn to apply sound clinical reasoning to any patient case they may encounter.

Derived from the best available evidence
Healer draws on current models of how clinical reasoning works, based on cognitive science. Case-based deliberate practice is central to the development of expertise as discussed by K. Anders Ericsson (Acad Med. 2015 Nov;90(11):1471-86). We’ve pulled from multiple sources to create the learning and assessments in Healer, central to which is illness script theory. These educational strategies are succinctly addressed by Dr. Judith L. Bowen’s powerful review article, Educational Strategies to Promote Clinical Diagnostic Reasoning (N Engl J Med 2006; 355:2217-2225). Dr. Bowen and other authors have recently updated and annotated this article with fresh perspective drawn from the intervening years of research on this topic. Download the article here.
Features
Introducing the most advanced way to teach, practice, and assess clinical reasoning skills
Data acquisition
Healer requires learners to gather clinical findings that they will use to justify their differential diagnosis during illness script building. Just like in the real world, there are lots of individual data points to sift through and lots of important follow-up questions to ask. Healer teaches the learner, in context, what questions are worth asking, what exams are worth performing, and what tests are worth ordering.
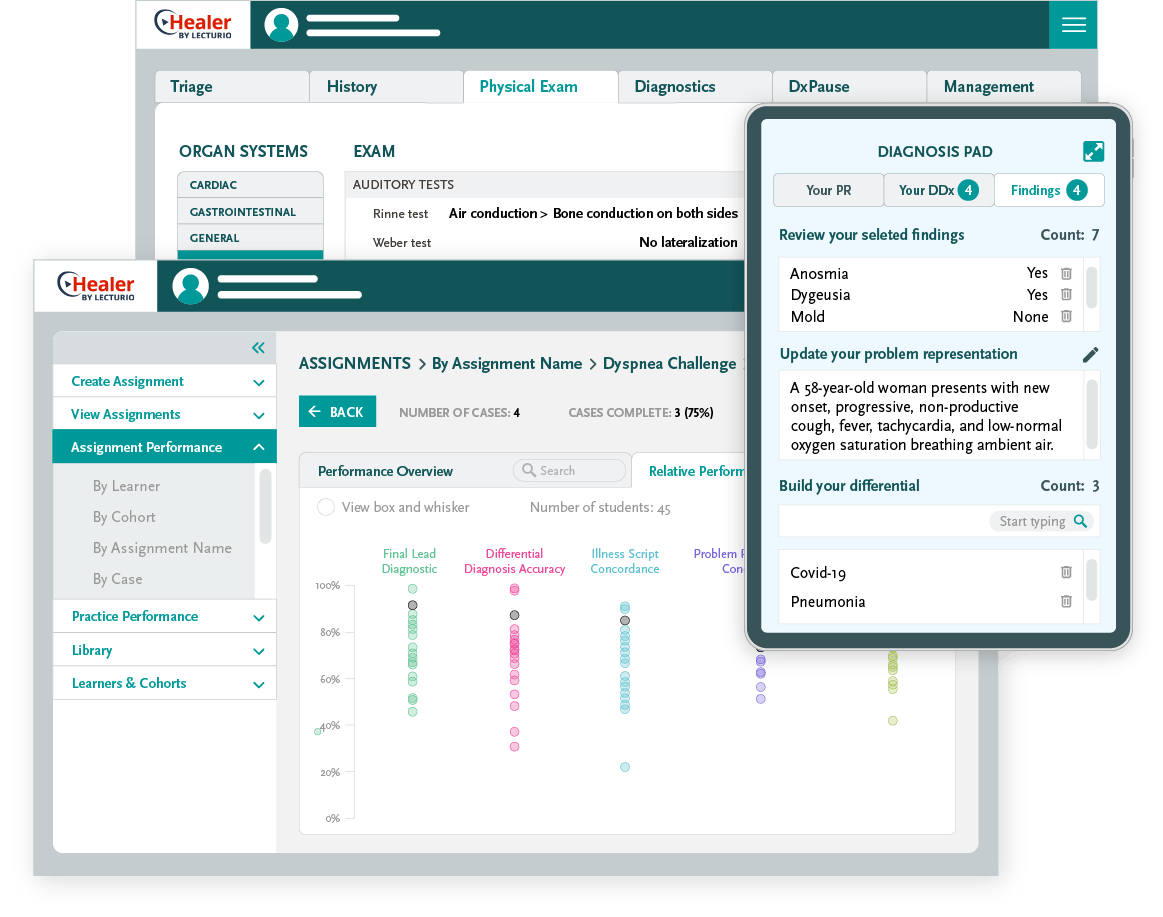
Problem representation and hypothesis-generation: The diagnosis pad
While the learner is reviewing data, they can do the work of reasoning in their Diagnosis Pad, where they can see the data they’ve selected as most important, create and modify their problem representation, and build their differential. As these are updated from stage to stage, they are saved for assessment and feedback in order to provide unique insights into the learner’s reasoning as it occurs.
Illness script building and differential diagnosis: The diagnostic pause
Once the learner has gathered the data, created their own problem representations and ranked their differential, they pause and build illness scripts for three diseases based on the expert’s selected data. Here, they reflect on which data in the case support or refute particular diseases and are able to see what questions, exams, and tests are crucial and which findings help to discriminate among likely diseases on the differential.
Performance assessment and feedback
Healer improves the evaluation of clinical reasoning with a proprietary, quantitative assessment that provides formative and summary performance scoring and detailed feedback on the learners’ clinical reasoning process and clinical knowledge. At a glance, learners receive objective assessment across 6 separate skills and perform informed self-assessment for two others. In the process, they can access the equivalent of hours’ worth of expert insight. The entire experience is self-directed, interactive, and engaging, motivating learners through focused repetition until they achieve mastery.
Experience a patient encounter yourself
Deliberate practice for developing sound clinical reasoning and achieving diagnostic excellence
Combining knowledge with deliberate practice
What makes a good doctor? What predicts real success?
It’s a combination of applied knowledge and solid clinical reasoning.
Because Healer exposes what and how experts think at each stage of the encounter, learners get the opportunity to experience and absorb the explicit and iterative steps of clinical reasoning while engaging in deliberate practice over time. They develop and improve their clinical knowledge, data acquisition, differential diagnostic abilities, and illness script instantiation all in the same platform, saving time for resource-strapped educators.
Gold-standard illness scripts and diagnostic schemas
Building illness scripts
Clinical expertise develops as clinicians combine experience with a particular disease and fundamental knowledge into their own illness scripts. Despite their central role in predicting diagnostic accuracy, illness scripts are rarely taught formally.
Working through each case, learners build illness scripts for a set of diseases on the expert’s differential, discovering which questions, exams, and tests are essential for a particular case. The exercise pushes learners to reflect on which data are most useful in differentiating one disease on their differential from others as well as the power of pertinent negatives.
Research
Experts call for improved clinical reasoning training in all phases of medical education

“Internal medicine clerkship directors believe that clinical reasoning should be taught throughout the 4 years of medical school, with the greatest emphasis in the clinical years. However, only a minority reported having teaching sessions devoted to clinical reasoning, citing a lack of curricular time and faculty expertise as the largest barriers. Our findings suggest that additional institutional and national resources should be dedicated to developing clinical reasoning curricula to improve diagnostic accuracy and reduce diagnostic error”1

“Learners should be encouraged to read about their patients’ problems in a way that promotes diagnostic reasoning, rather than to read about topics in a rote-memorization fashion, without context. The organization of knowledge stored in memory facilitates the recall of key concepts for application to the next relevant clinical case.”2

“Diagnostic errors cause substantial preventable harm. In a 2019 study published in the journal Diagnosis, “Causes were disproportionately clinical judgment factors (85.7%) across categories (range 82.0–88.8%).”3

“From a National Survey of Internal Medicine Clerkship Directors Most respondents reported that a structured curriculum in clinical reasoning should be taught in all phases of medical education, including the preclinical years (64/85; 75%), clinical clerkships (76/87; 87%), and the fourth year (75/88; 85%), and that more curricular time should be devoted to the topic.” “Respondents indicated that most students enter the clerkship with only poor (25/85; 29%) to fair (47/85; 55%) knowledge of key clinical reasoning concepts. Most institutions (52/91; 57%) surveyed lacked sessions dedicated to these topics. Lack of curricular time (59/67, 88%) and faculty expertise in teaching these concepts (53/76, 69%) were identified as barriers.”4

“A case vignette-based clinical reasoning curriculum can effectively increase residents’ knowledge of clinical reasoning concepts and their self-assessed ability to recognize and apply clinical reasoning concepts.”5

“Background Errors in medicine are common and often tied to diagnosis. Educating physicians about the science of cognitive decision-making, especially during medical school and residency when trainees are still forming clinical habits, may enhance awareness of individual cognitive biases and has the potential to reduce diagnostic errors and improve patient safety.”6

“Diagnostic reasoning deficits are frequently identified in students and residents referred for remediation. Effective remediation of diagnostic reasoning deficits includes both granular assessment of the learner’s diagnostic reasoning pathway—from hypothesis generation to working diagnosis—and targeted coaching exercises for the learner (along with their pedagogical purpose).”7
- Dozens of virtual patient encounters
- Expert problem representations, management plans, differential diagnoses, and rationales to help guide learners
- Hundreds of diseases to consider
- An overview of clinical reasoning and a glossary of key terms
- 100+ expert illness scripts to provide and support students’ clinical knowledge
- Detailed assessment of clinical reasoning skills
Experience a patient encounter yourself
Schedule a Healer demonstration and see how easy it is to integrate science-based clinical reasoning curriculum development and assessment into your program.