Volume status is a balance between water and solutes, the majority of which is Na. Volume depletion (also known as hypovolemia) refers to a loss of both water and Na, whereas dehydration refers only to a loss of water. Dehydration is primarily caused by decreased water intake and presents with increased thirst and can progress to altered mental status and low blood pressure if severe. Volume depletion can be caused by GI losses, renal losses, bleeding, poor oral Na intake, or third spacing of fluids. The clinical presentation has relatively nonspecific symptoms but will ultimately cause low blood pressure if severe. The diagnosis of these imbalances is based on lab findings in addition to clinical symptoms and signs, which can be subtle and unreliable. Management requires differentiation between these 2 conditions. The treatment is to administer fluids with tonicity similar to those lost; isotonic fluids are used for volume depletion, and hypotonic fluids are used for dehydration.
Last updated: Dec 15, 2025
Dehydration refers only to a loss of water, while volume depletion refers to a loss of both water and Na+.
The relative differences between losses of water and Na determine how water shifts between the fluid compartments of the body. With volume depletion and dehydration, there are fluid shifts between the compartments.
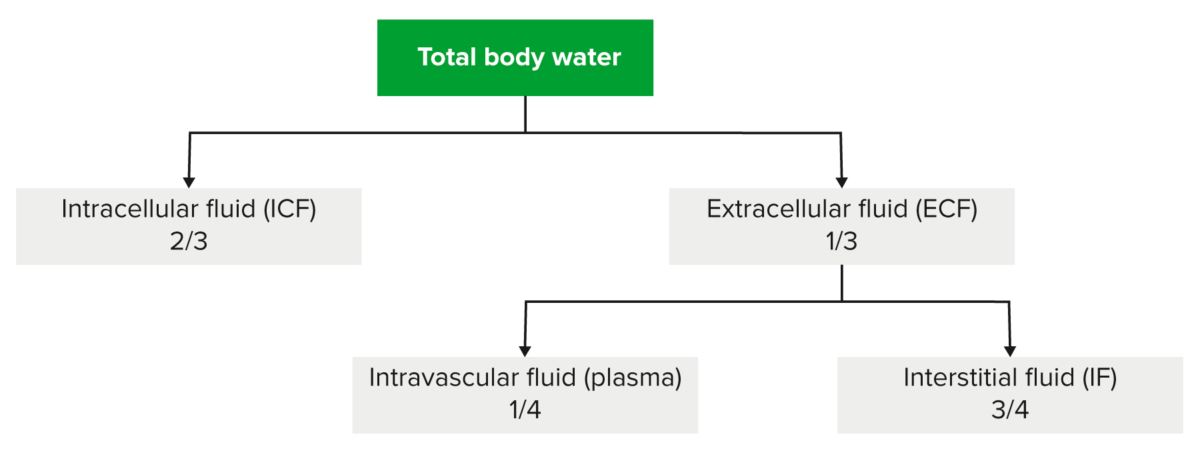
Distribution of total body water within the body
Image by Lecturio.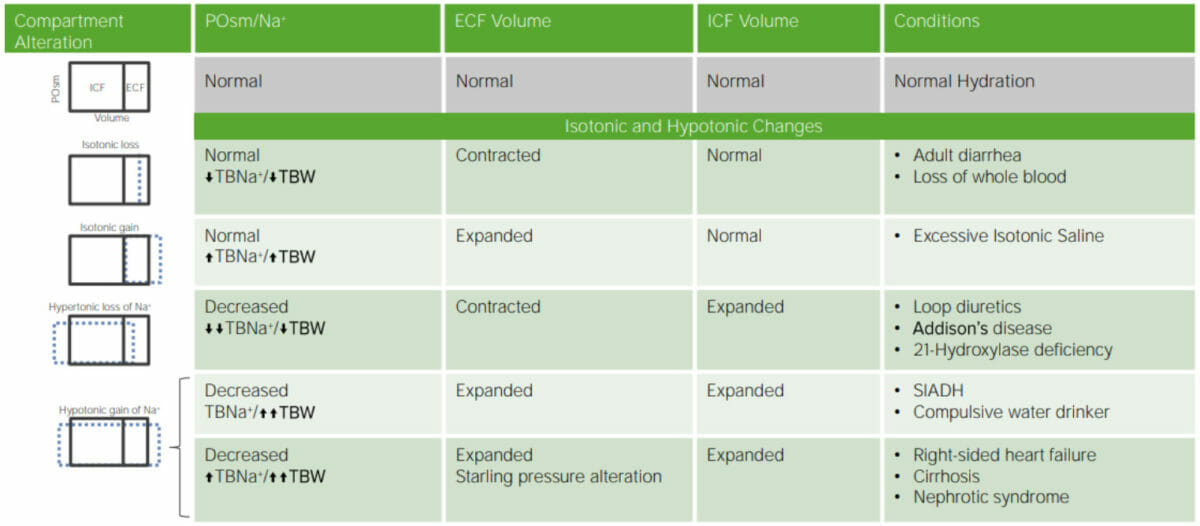
Dehydration: Summary of Isotonic and Hypotonic.
BNa+= total body sodium
SIADH = syndrome of inappropriate antidiuretic hormone secretion
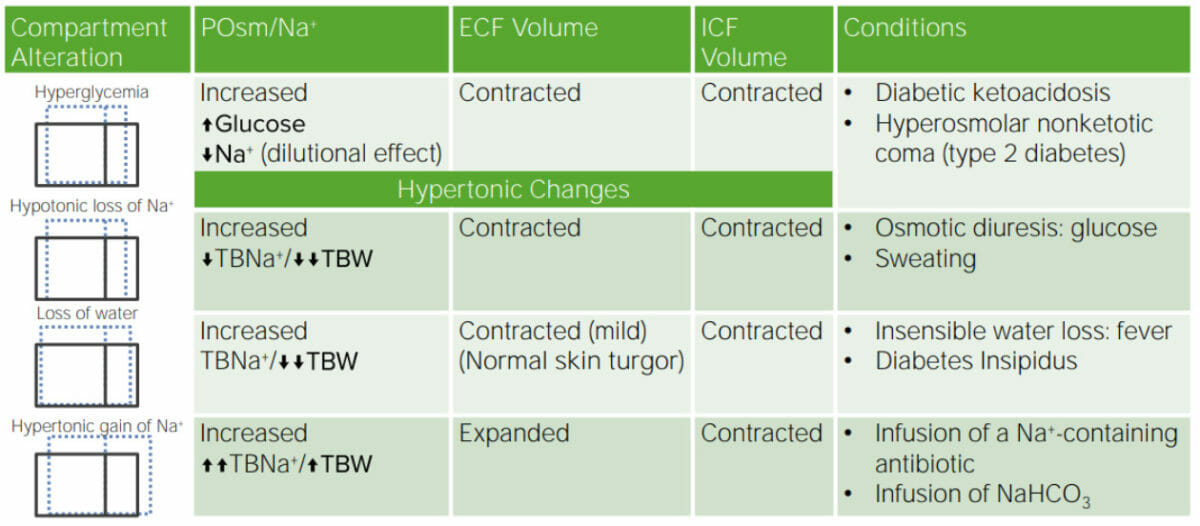
Review of disorders of water and Na
NaHCO3: sodium bicarbonate
The clinical presentation of dehydration and volume depletion varies greatly depending on the severity, from asymptomatic to potentially fatal hypovolemic shock Hypovolemic Shock Types of Shock.
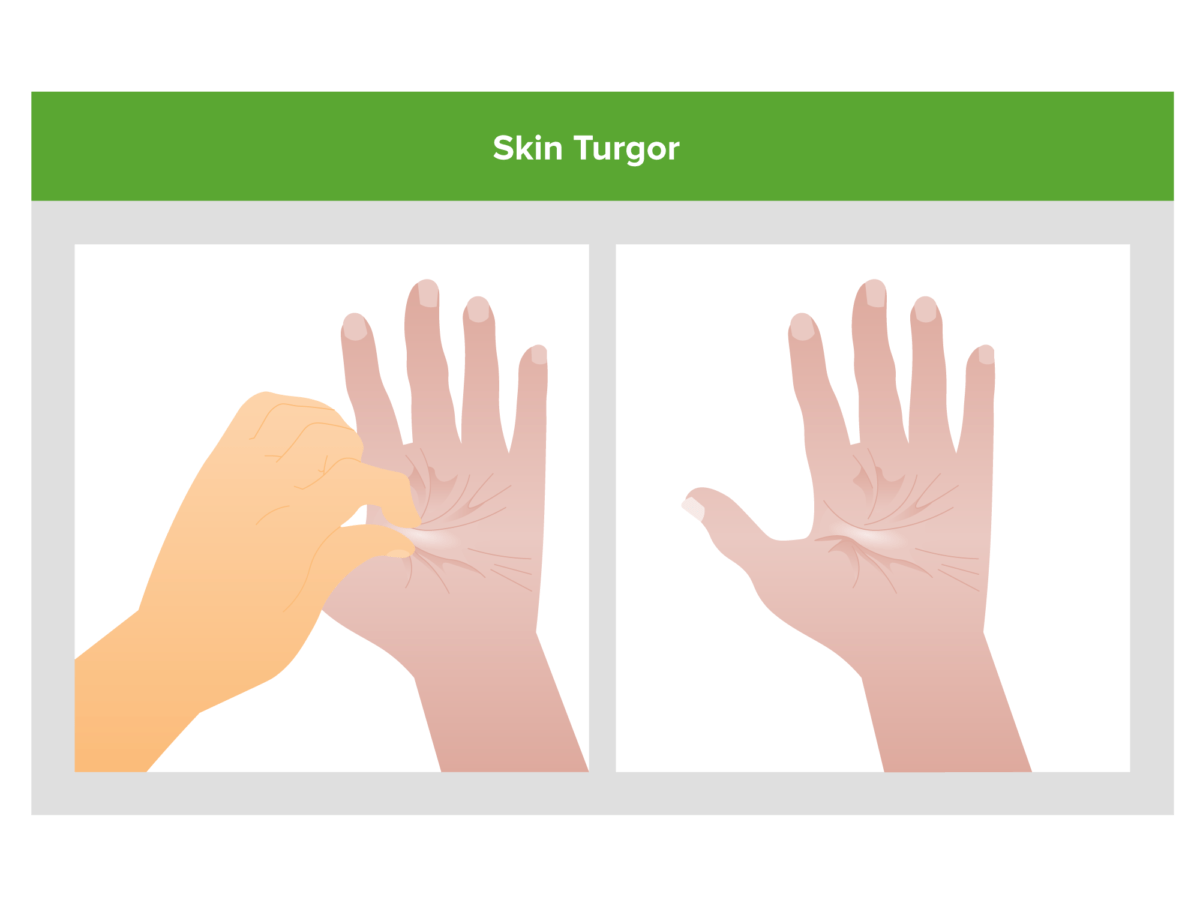
Decreased skin turgor (i.e., skin tenting when pinched):
A sign of decreased total body Na+.
Determining the volume status Volume Status ACES and RUSH: Resuscitation Ultrasound Protocols is often challenging, and the history, physical exam, and lab results must be integrated. Outside of extremes, signs and symptoms of dehydration are subtle and unreliable and should not be used alone for detecting dehydration and volume depletion.
The primary management of hypovolemia Hypovolemia Sepsis in Children is to replace the fluids lost with similar tonicity Tonicity Plasma tonicity refers to the concentration of only the osmotically active solutes in blood Renal Sodium and Water Regulation of fluids; electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes must also be monitored.
In hypertonic Hypertonic Solutions that have a greater osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation dehydration, the loss of water from the body is greater than the loss of electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes ( sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia, potassium Potassium An element in the alkali group of metals with an atomic symbol k, atomic number 19, and atomic weight 39. 10. It is the chief cation in the intracellular fluid of muscle and other cells. Potassium ion is a strong electrolyte that plays a significant role in the regulation of fluid volume and maintenance of the water-electrolyte balance. Hyperkalemia, etc ETC The electron transport chain (ETC) sends electrons through a series of proteins, which generate an electrochemical proton gradient that produces energy in the form of adenosine triphosphate (ATP). Electron Transport Chain (ETC).). As a result, the ECF becomes more concentrated, with an increased osmolarity Osmolarity The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per liter of solution. Osmolality is expressed in terms of osmoles of solute per kilogram of solvent. Hypernatremia. Symptoms of hypertonic Hypertonic Solutions that have a greater osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation dehydration may include extreme thirst, dry mucous membranes (dry mouth), dark urine, sunken eyes Sunken eyes Rotavirus, and altered mental status Altered Mental Status Sepsis in Children. It can also lead to hypernatremia Hypernatremia Hypernatremia is an elevated serum sodium concentration > 145 mmol/L. Serum sodium is the greatest contributor to plasma osmolality, which is very tightly controlled by the hypothalamus via the thirst mechanism and antidiuretic hormone (ADH) release. Hypernatremia occurs either from a lack of access to water or an excessive intake of sodium. Hypernatremia (high blood sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia levels).
The term hypotonic Hypotonic Solutions that have a lesser osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation dehydration refers to a loss of electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes (especially sodium Sodium A member of the alkali group of metals. It has the atomic symbol na, atomic number 11, and atomic weight 23. Hyponatremia) from the body that exceeds the loss of water. This results in the ECF becoming less concentrated, with a decreased osmolarity Osmolarity The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per liter of solution. Osmolality is expressed in terms of osmoles of solute per kilogram of solvent. Hypernatremia. Symptoms of hypotonic Hypotonic Solutions that have a lesser osmotic pressure than a reference solution such as blood, plasma, or interstitial fluid. Renal Sodium and Water Regulation dehydration may include nausea Nausea An unpleasant sensation in the stomach usually accompanied by the urge to vomit. Common causes are early pregnancy, sea and motion sickness, emotional stress, intense pain, food poisoning, and various enteroviruses. Antiemetics, vomiting Vomiting The forcible expulsion of the contents of the stomach through the mouth. Hypokalemia, muscle cramps Cramps Ion Channel Myopathy, weakness, lethargy Lethargy A general state of sluggishness, listless, or uninterested, with being tired, and having difficulty concentrating and doing simple tasks. It may be related to depression or drug addiction. Hyponatremia, and in severe cases, cerebral edema Cerebral edema Increased intracellular or extracellular fluid in brain tissue. Cytotoxic brain edema (swelling due to increased intracellular fluid) is indicative of a disturbance in cell metabolism, and is commonly associated with hypoxic or ischemic injuries. An increase in extracellular fluid may be caused by increased brain capillary permeability (vasogenic edema), an osmotic gradient, local blockages in interstitial fluid pathways, or by obstruction of CSF flow (e.g., obstructive hydrocephalus). Increased Intracranial Pressure (ICP) ( swelling Swelling Inflammation of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification).
Isotonic Isotonic Solutions having the same osmotic pressure as blood serum, or another solution with which they are compared. Renal Sodium and Water Regulation dehydration means that there is an equal loss of both water and electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes from the body, maintaining the normal osmolarity Osmolarity The concentration of osmotically active particles in solution expressed in terms of osmoles of solute per liter of solution. Osmolality is expressed in terms of osmoles of solute per kilogram of solvent. Hypernatremia of the ECF. Symptoms of isotonic Isotonic Solutions having the same osmotic pressure as blood serum, or another solution with which they are compared. Renal Sodium and Water Regulation dehydration may include dry skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions, dry mouth, sunken fontanelle Fontanelle Any of six membrane-covered openings between the cranial sutures in the incompletely ossified skull of the fetus or newborn infant. The fontanelles normally close sometime after birth. Skull: Anatomy in infants, decreased urine output, and overall signs of mild to moderate dehydration Moderate Dehydration Fluid Replacement Therapy in Children.