Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology transport deoxygenated blood and waste products from capillaries Capillaries Capillaries are the primary structures in the circulatory system that allow the exchange of gas, nutrients, and other materials between the blood and the extracellular fluid (ECF). Capillaries are the smallest of the blood vessels. Because a capillary diameter is so small, only 1 RBC may pass through at a time. Capillaries: Histology in the periphery back to the heart. Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology are capacitance vessels Capacitance vessels Veins: Histology, meaning that they can stretch significantly, increasing the volume of fluid they can hold without significantly increasing their pressure. Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology respond to stimulation from the ANS ANS The ans is a component of the peripheral nervous system that uses both afferent (sensory) and efferent (effector) neurons, which control the functioning of the internal organs and involuntary processes via connections with the CNS. The ans consists of the sympathetic and parasympathetic nervous systems. Autonomic Nervous System: Anatomy, as arteries Arteries Arteries are tubular collections of cells that transport oxygenated blood and nutrients from the heart to the tissues of the body. The blood passes through the arteries in order of decreasing luminal diameter, starting in the largest artery (the aorta) and ending in the small arterioles. Arteries are classified into 3 types: large elastic arteries, medium muscular arteries, and small arteries and arterioles. Arteries: Histology do, but to less of an extent. The effects of either venoconstriction or venodilation, however, impact venous capacitance. As veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology constrict, capacitance goes down, forcing more blood back to the heart (i.e., increasing venous return), which in turn affects the amount of blood that can be pumped out of the heart on the next heartbeat. Thus, changes in venous capacitance can significantly affect cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics (CO). These effects can be plotted on graphs known as venous function curves.
Last updated: Dec 15, 2025
Veins Veins Veins are tubular collections of cells, which transport deoxygenated blood and waste from the capillary beds back to the heart. Veins are classified into 3 types: small veins/venules, medium veins, and large veins. Each type contains 3 primary layers: tunica intima, tunica media, and tunica adventitia. Veins: Histology are tubular collections of cells that transport deoxygenated blood and waste products from capillaries Capillaries Capillaries are the primary structures in the circulatory system that allow the exchange of gas, nutrients, and other materials between the blood and the extracellular fluid (ECF). Capillaries are the smallest of the blood vessels. Because a capillary diameter is so small, only 1 RBC may pass through at a time. Capillaries: Histology in the periphery of the body back to the heart.
Pressure in the venous system is too low to spontaneously push blood against gravity; moving blood against gravity up to the heart requires:
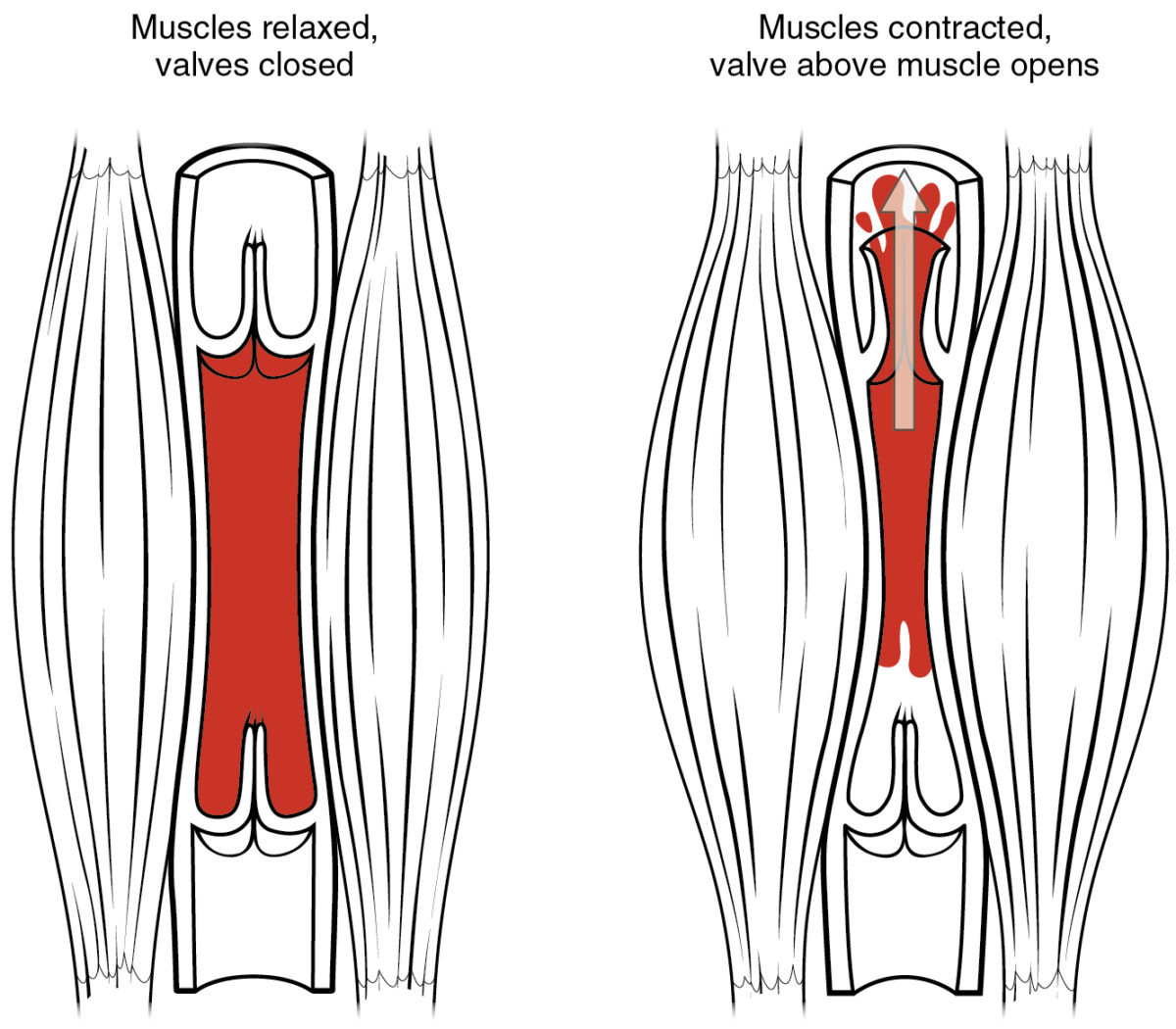
Muscle pump and venous valves:
As skeletal muscles surrounding a vein contract, they compress the vessel, forcing the blood to move forward. One-way valves within the veins prevent back-flow and ensures blood only flows in one direction.
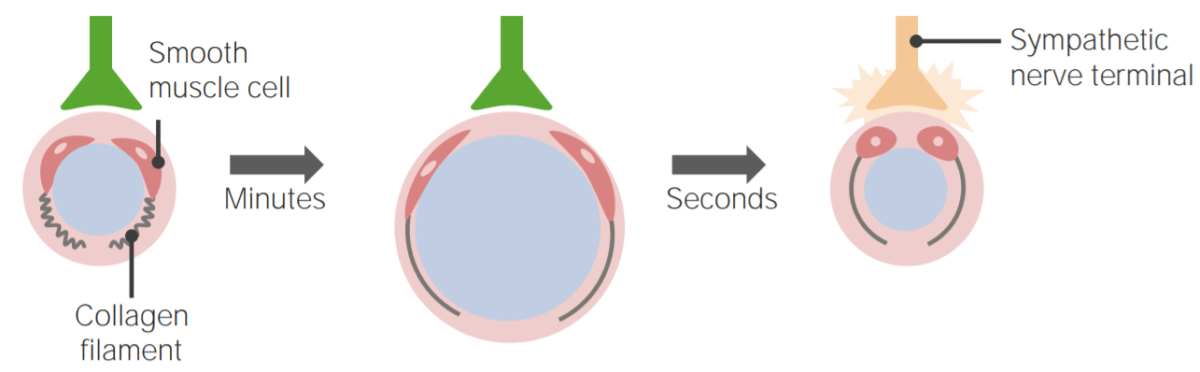
Venous pressure:
Smooth muscle in vein walls can contract or relax, changing the luminal diameter within a vein. Sympathetic stimulation causes venoconstriction, reducing venous capacitance and forcing more blood back to the heart. This increases preload, which in turn can increase stroke volume and cardiac output (CO).
Venous function curves (also known as systemic vascular function curves) plot central venous pressure Central venous pressure The blood pressure in the central large veins of the body. It is distinguished from peripheral venous pressure which occurs in an extremity. Central Venous Catheter ( CVP CVP The blood pressure in the central large veins of the body. It is distinguished from peripheral venous pressure which occurs in an extremity. Central Venous Catheter) against CO.
Cardiac output Cardiac output The volume of blood passing through the heart per unit of time. It is usually expressed as liters (volume) per minute so as not to be confused with stroke volume (volume per beat). Cardiac Mechanics:
Central venous pressure Central venous pressure The blood pressure in the central large veins of the body. It is distinguished from peripheral venous pressure which occurs in an extremity. Central Venous Catheter:
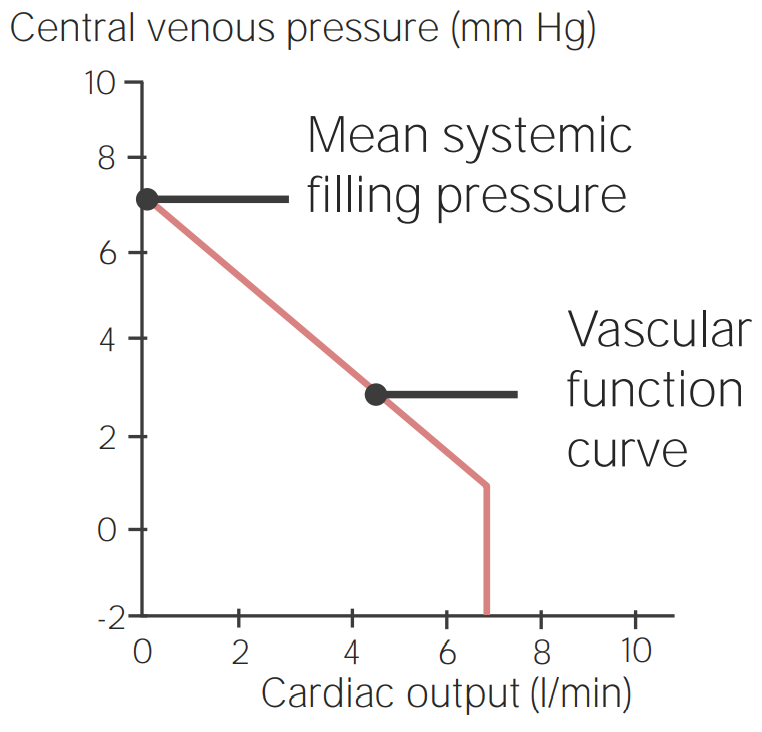
Example of a venous function curve:
Central venous pressure (CVP) is plotted along the Y-axis and cardiac output (CO) is plotted on the X-axis. There is an inverse linear relationship between the 2 variables until a CO is reached, at which point CVP drops to 0 (because veins have the ability to collapse).
Venous function curve shape:
Mean systemic filling pressure (mean circulatory pressure)
Factors affecting the shape/location of the curve:
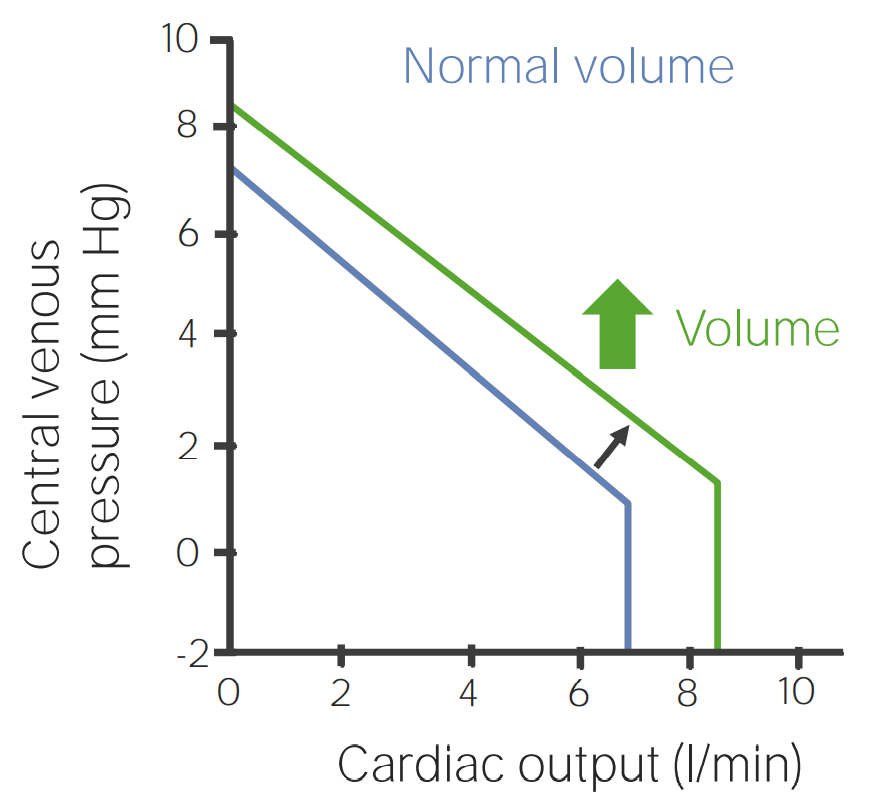
Venous function curve when blood volume increases
Image by Lecturio.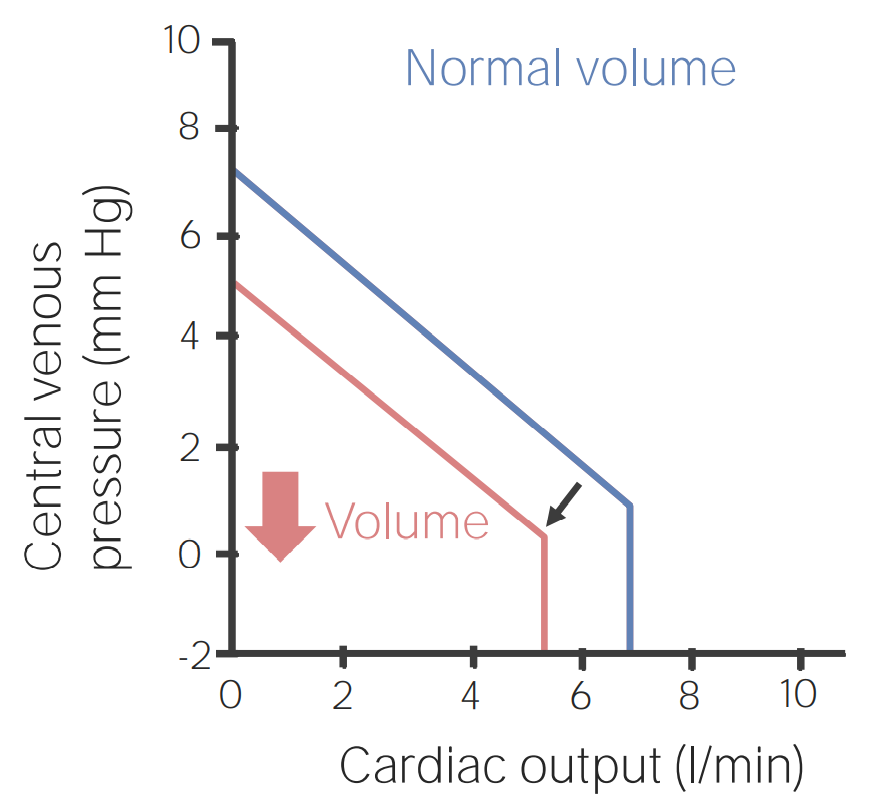
Venous function curve when blood volume decreases
Image by Lecturio.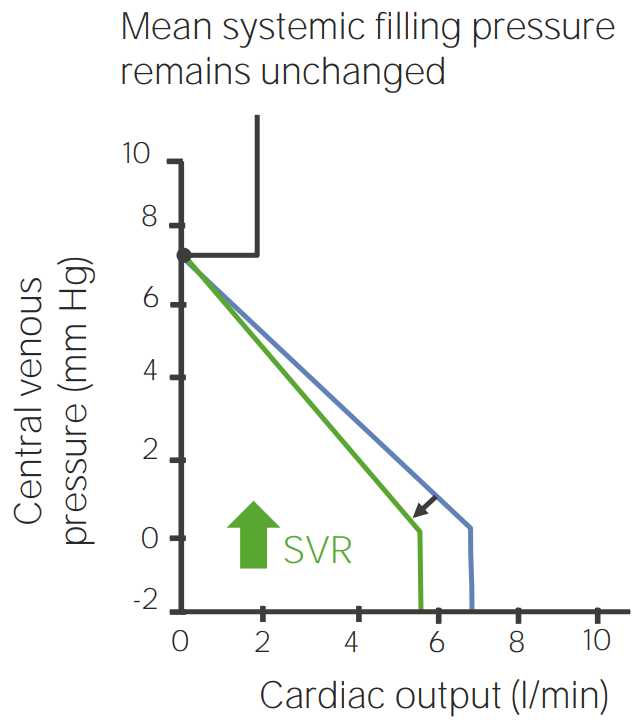
Venous function curve showing the effects of systemic vascular resistance (SVR) increasing
Image by Lecturio.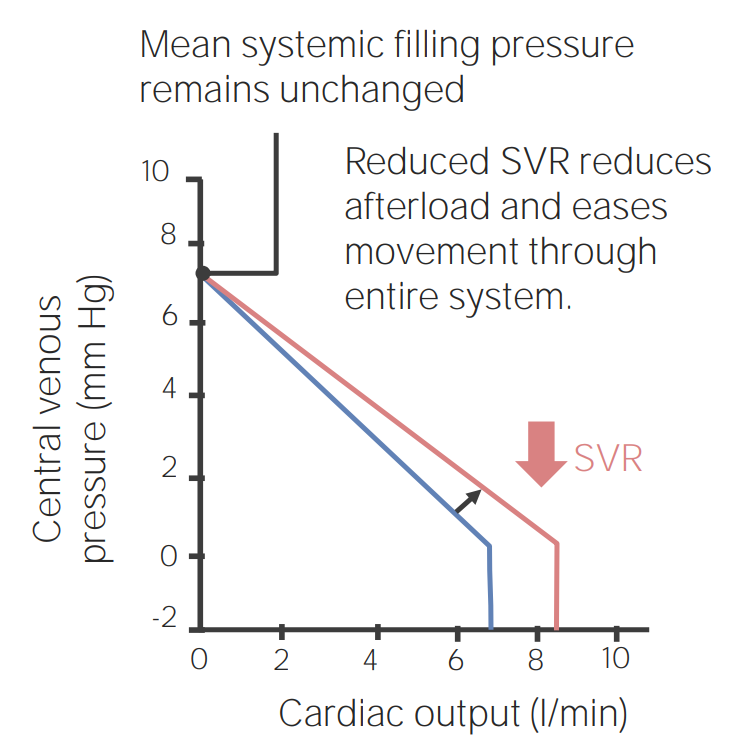
Venous function curve showing the effects of systemic vascular resistance (SVR) decreasing
Image by Lecturio.Venoconstriction:
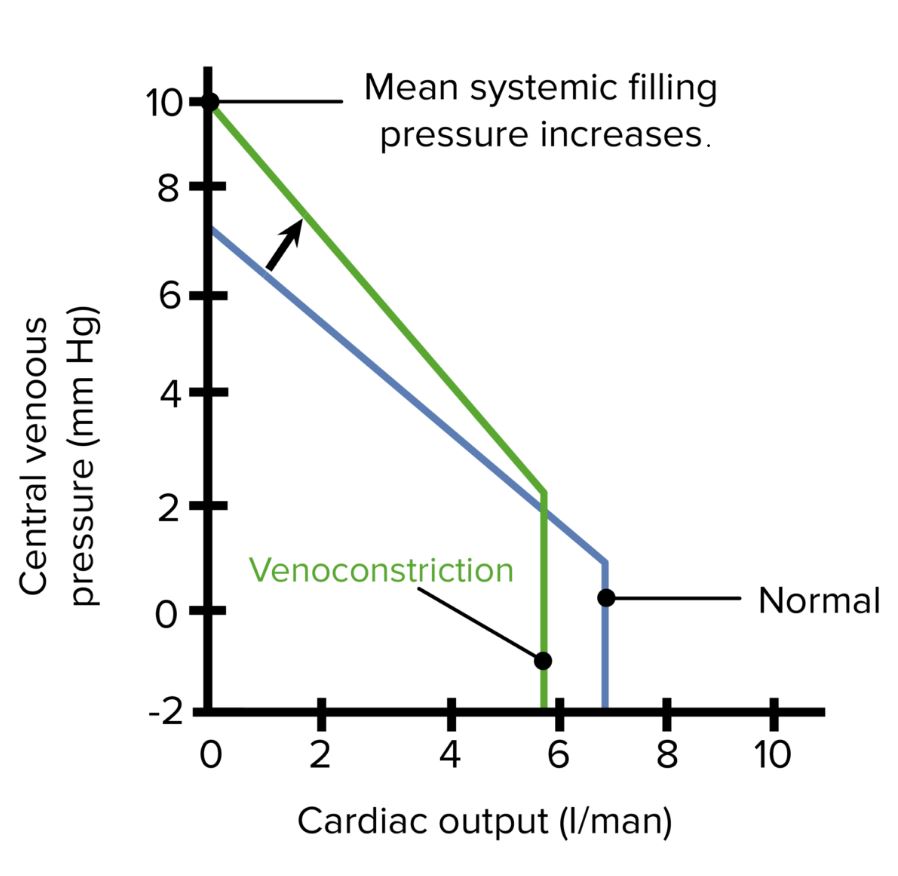
Venous function curve showing the effects of venoconstriction
Image by Lecturio.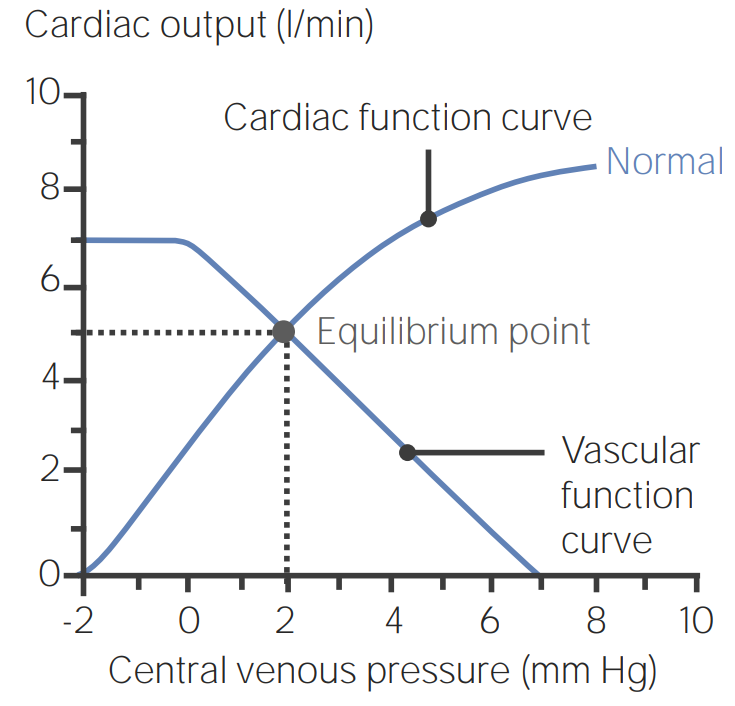
Combined venous/cardiac function curve illustrating the equilibrium point between central venous pressure (CVP) and cardiac output (CO):
A CVP of 2 mm Hg and a CO of 5 L/min is the functional average for most people.
Clinical scenario #1: MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction leading to a decrease in inotropy
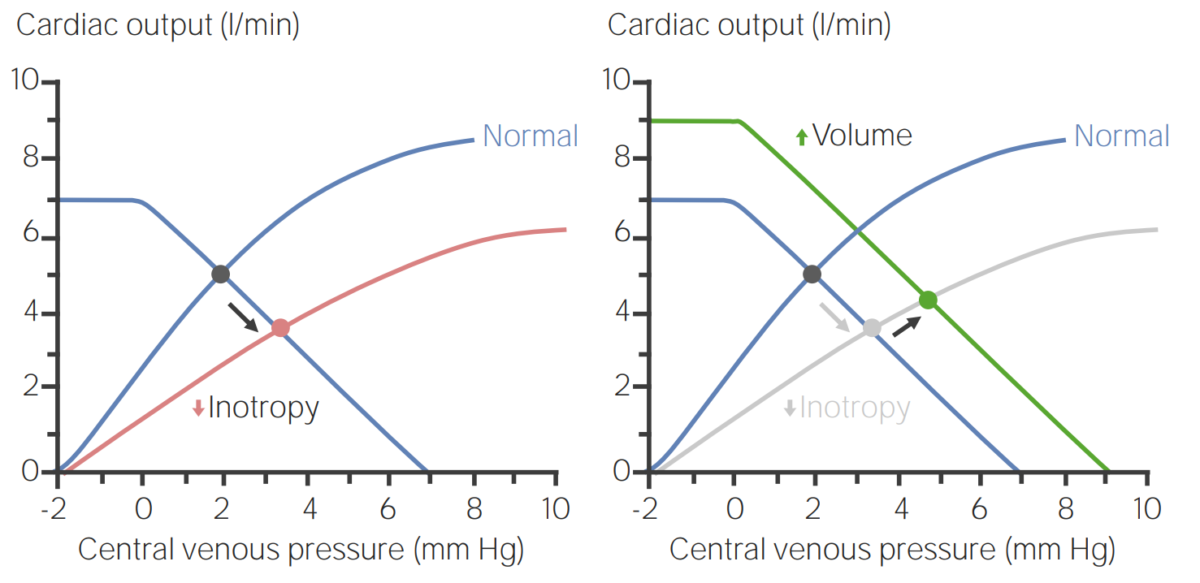
Venous function curves illustrating how the body can increase blood volume to compensate for a decrease in inotropy:
(Left) When inotropy is decreased, central venous pressure (CVP) increases, whereas cardiac output (CO) decreases. However, expanding the intravascular volume can compensate for these changes to improve CO (right).
Clinical scenario #2: hemorrhage
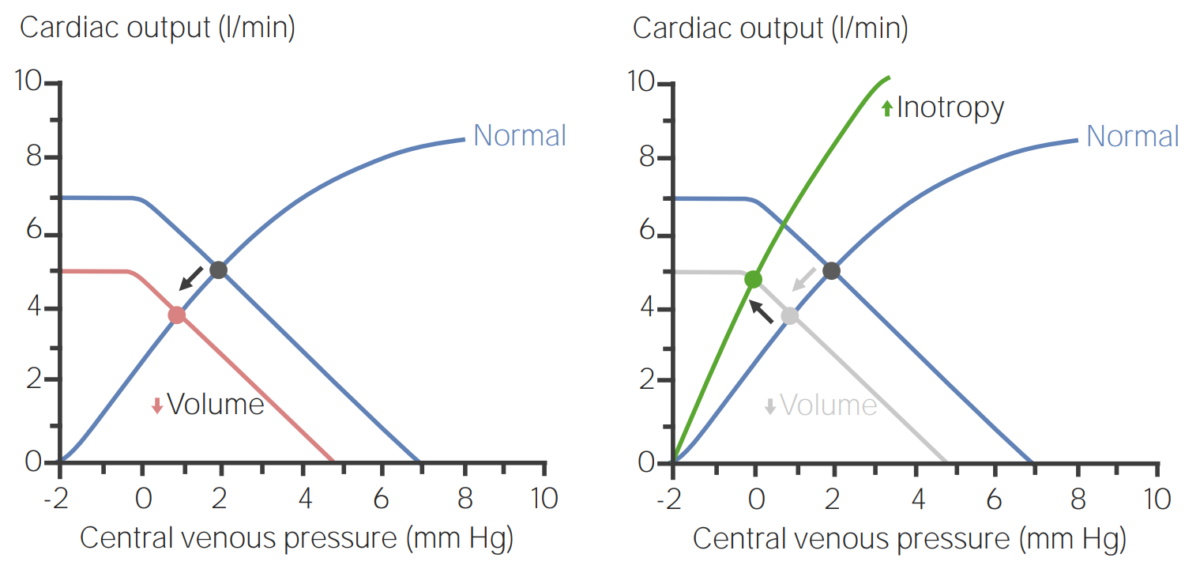
Venous function curves illustrating how an increase in inotropy (i.e., contractility) compensates for a decrease in blood volume:
(Left) When volume is decreased, central venous pressure (CVP) decreases along with cardiac output (CO). However, increasing inotropy can compensate for these changes to improve CO (right).