Hypertension is defined as a blood pressure (BP) of ≥130/80 mm Hg. Significantly elevated BP (≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic) carries a substantial risk of morbidity and mortality. Despite the prolonged presence of hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, there may be no signs or symptoms of end-organ damage (e.g., brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, eyes, heart, kidneys Kidneys The kidneys are a pair of bean-shaped organs located retroperitoneally against the posterior wall of the abdomen on either side of the spine. As part of the urinary tract, the kidneys are responsible for blood filtration and excretion of water-soluble waste in the urine. Kidneys: Anatomy) until function becomes decompensated or severely impaired. Individuals may present with clinical symptoms such as chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways due to MI MI MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction or focal neurologic changes associated with a cerebral infarction or intracranial hemorrhage Intracranial hemorrhage Subarachnoid hemorrhage (SAH) is a type of cerebrovascular accident (stroke) resulting from intracranial hemorrhage into the subarachnoid space between the arachnoid and the pia mater layers of the meninges surrounding the brain. Most sahs originate from a saccular aneurysm in the circle of willis but may also occur as a result of trauma, uncontrolled hypertension, vasculitis, anticoagulant use, or stimulant use. Subarachnoid Hemorrhage. Diagnosis is made using serial blood pressure measurements and testing for end-organ damage. Management includes lowering the blood pressure and treating specific organ damage.
Last updated: Dec 15, 2025
Regardless of the manifestation of severe hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, by definition, the individual will have a blood pressure ≥ 180 mm Hg systolic and/or ≥ 120 mm Hg diastolic.
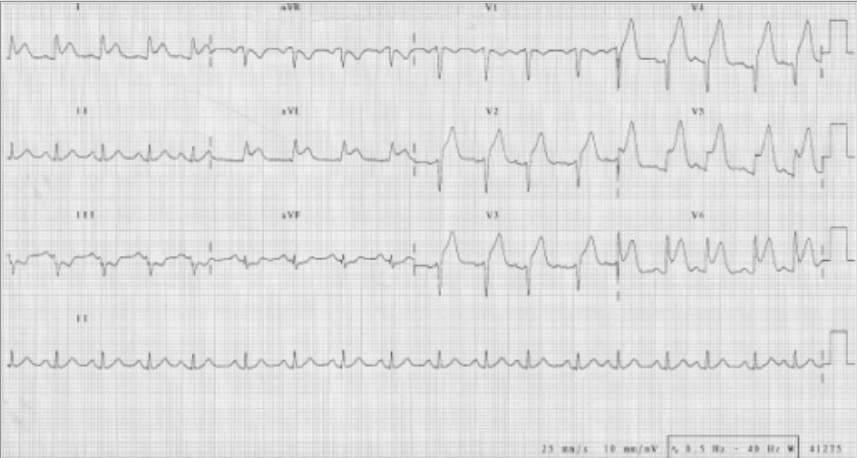
ECG indicating an anterior MI with ST-segment elevations seen in leads V2‒V6, I, and aVL:
Also note the reciprocal ST depressions in III and aVF.

Subarachnoid hemorrhage:
CT scan showing intracranial bleeding
During the initial assessment of an individual with severe hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, it is imperative to exclude chronic target-organ damage. Severe elevations in blood pressure should be quickly confirmed with repeat measurement.
Particular focus on risk factors for end-organ vascular events:
Symptoms of end-organ dysfunction:
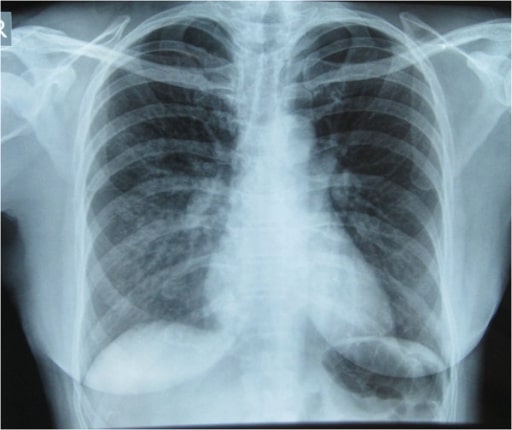
Chest X-ray showing pulmonary infiltrates in the right lung, especially in the right middle and lower lung zones, which are indicative of pulmonary edema
Image: “Initial Chest x-ray” by Nepal International Clinic, Travel and Mountain Medicine, Kathmandu, Nepal. License: CC BY 2.0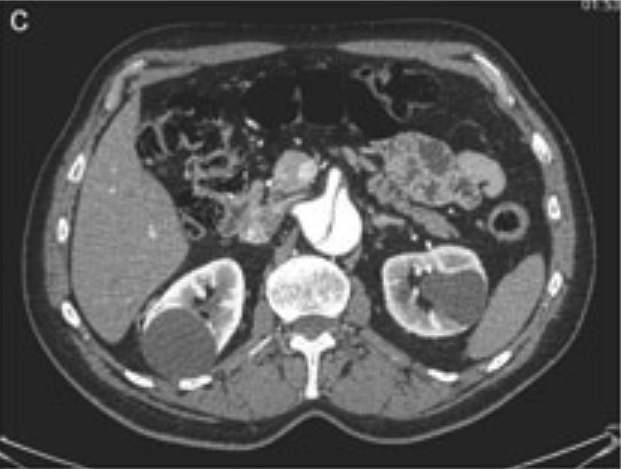
CT scan showing abdominal aortic dissection
Image: “Aortic dissection identified in the contrast-enhanced CT scan” by Department of Medical, Surgical and Neuro Sciences, Section of Radiological Sciences, Siena, Italy. License: CC BY 2.0, cropped by Lecturio.Outpatient management:
ED management: