Ulcerative colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis (UC) is an idiopathic Idiopathic Dermatomyositis inflammatory condition that involves the mucosal surface of the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy. It is a type of inflammatory bowel disease (IBD), along with Crohn's disease (CD). The rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy is always involved, and inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation may extend proximally through the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy. Ulcerative colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis causes diffuse friability, erosions Erosions Corneal Abrasions, Erosion, and Ulcers with bleeding, and loss of haustra Haustra Colon, Cecum, and Appendix: Anatomy, which are visible on endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD). Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with bloody diarrhea Bloody diarrhea Diarrhea, colicky abdominal pain Abdominal Pain Acute Abdomen, tenesmus, and fecal urgency. Diagnosis is established via endoscopy Endoscopy Procedures of applying endoscopes for disease diagnosis and treatment. Endoscopy involves passing an optical instrument through a small incision in the skin i.e., percutaneous; or through a natural orifice and along natural body pathways such as the digestive tract; and/or through an incision in the wall of a tubular structure or organ, i.e. Transluminal, to examine or perform surgery on the interior parts of the body. Gastroesophageal Reflux Disease (GERD) with biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma and by ruling out other causes of bloody diarrhea Bloody diarrhea Diarrhea. Management is primarily through topical mesalamine, 6-mercaptopurine 6-Mercaptopurine An antimetabolite antineoplastic agent with immunosuppressant properties. It interferes with nucleic acid synthesis by inhibiting purine metabolism and is used, usually in combination with other drugs, in the treatment of or in remission maintenance programs for leukemia. Antimetabolite Chemotherapy, or colectomy for severe cases. Complications include fulminant colitis Fulminant colitis Pseudomembranous Colitis, toxic megacolon Toxic megacolon An acute form of megacolon, severe pathological dilatation of the colon. It is associated with clinical conditions such as ulcerative colitis; Crohn disease; amebic dysentery; or Clostridium enterocolitis. Megacolon, intestinal perforation Intestinal perforation Perforated viscus or GI perforation represents a condition in which the integrity of the GI wall is lost with subsequent leakage of enteric contents into the peritoneal cavity, resulting in peritonitis. The causes of perforated viscus include trauma, bowel ischemia, infections, or ulcerative conditions, all of which ultimately lead to a full-thickness disruption of the intestinal wall. Perforated Viscus, and increased risk of colorectal cancer Colorectal cancer Colorectal cancer (CRC) is the 2nd leading cause of cancer-related deaths in the United States. Colorectal cancer is a heterogeneous disease that arises from genetic and epigenetic abnormalities, with influence from environmental factors. Colorectal Cancer.
Last updated: Dec 15, 2025
An increased risk of developing ulcerative colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis (UC) may be associated with the following:
The exact pathophysiology is unknown, but is likely associated with a combination of dysregulation of the intestinal epithelium Epithelium The epithelium is a complex of specialized cellular organizations arranged into sheets and lining cavities and covering the surfaces of the body. The cells exhibit polarity, having an apical and a basal pole. Structures important for the epithelial integrity and function involve the basement membrane, the semipermeable sheet on which the cells rest, and interdigitations, as well as cellular junctions. Surface Epithelium: Histology and the immune system Immune system The body’s defense mechanism against foreign organisms or substances and deviant native cells. It includes the humoral immune response and the cell-mediated response and consists of a complex of interrelated cellular, molecular, and genetic components. Primary Lymphatic Organs.
The inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation invariably involves the rectum Rectum The rectum and anal canal are the most terminal parts of the lower GI tract/large intestine that form a functional unit and control defecation. Fecal continence is maintained by several important anatomic structures including rectal folds, anal valves, the sling-like puborectalis muscle, and internal and external anal sphincters. Rectum and Anal Canal: Anatomy and may extend proximally through the colon Colon The large intestines constitute the last portion of the digestive system. The large intestine consists of the cecum, appendix, colon (with ascending, transverse, descending, and sigmoid segments), rectum, and anal canal. The primary function of the colon is to remove water and compact the stool prior to expulsion from the body via the rectum and anal canal. Colon, Cecum, and Appendix: Anatomy in a continuous fashion.
The typical presentation for UC is a relapsing disorder that includes the following:
| Features | Mild | Moderate | Severe |
|---|---|---|---|
| Stool frequency per day | < 4 | 4–6 | > 6 |
| Symptoms |
|
|
|
| Systemic toxicity Toxicity Dosage Calculation | Normal findings:
|
Laboratory abnormalities:
|
Laboratory abnormalities:
|
| Erythrocyte sedimentation rate Erythrocyte Sedimentation Rate Soft Tissue Abscess ( ESR ESR Soft Tissue Abscess) | < 20 | 20–30 | > 30 |
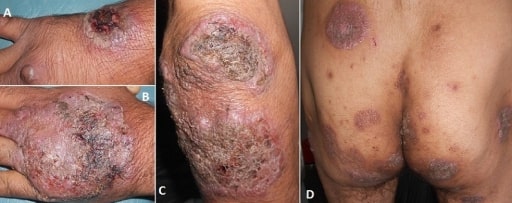
Pyoderma gangrenosum
Image: “Vegetating idiopathic pyoderma gangrenosum” by Service de Dermatologie, CHU Ibn Sina, Rabat, Maroc. License: CC BY 2.0Laboratory studies:
Stool studies: may be used to exclude other causes of inflammatory diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea (e.g., infection)
Abdominal imaging:
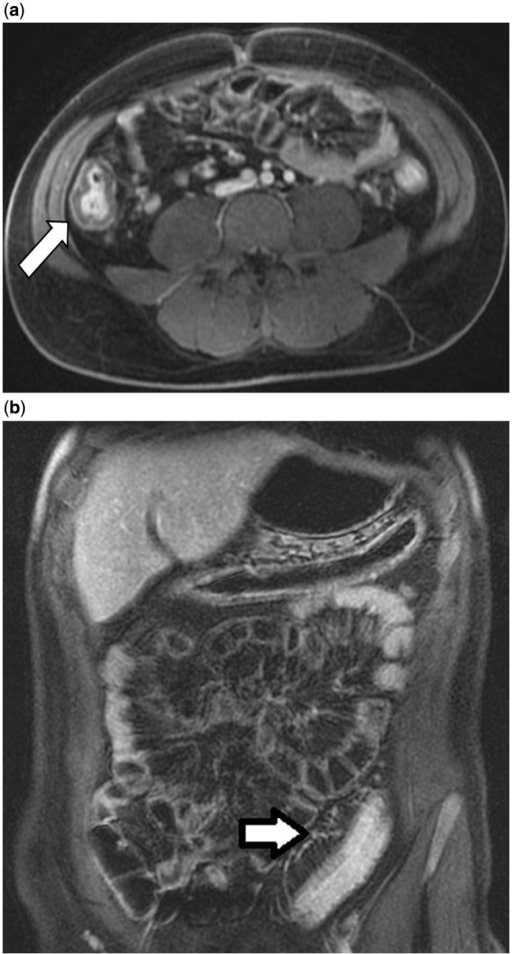
Magnetic resonance enterography in a 24-year-old male with ulcerative colitis. 4a: Colonic wall thickening (white arrow) and hyperenhancement of the right colon. 4b: Engorgement of the pericolonic vasa recta (white arrow) with colonic wall thickening and hyperenhancement in the sigmoid colon.
Image: “Magnetic resonance enterography” by Division of Gastroenterology and Hepatology, Mayo Clinic College of Medicine, Rochester MN, USA. License: CC BY 3.0
Double-contrast barium enema illustrating granular mucosa in a patient with active ulcerative colitis
Image: “Double contrast barium enema” by Division of Gastroenterology and Hepatology, Mayo Clinic College of Medicine, Rochester MN, USA. License: CC BY 3.0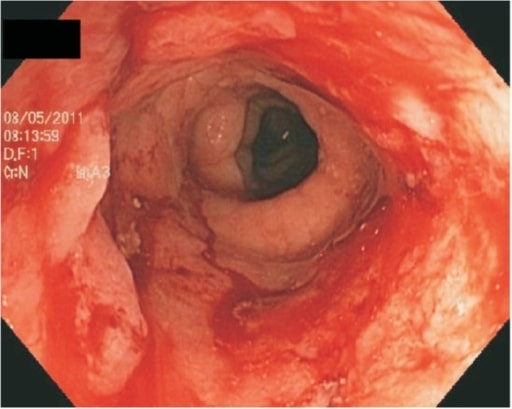
Endoscopic view of the colon showing continuous ulceration due to severe ulcerative colitis
Image: “Ulcerative proctitis” by G.V. (Sonny) Montgomery VA Medical Center and Division of Digestive Diseases, Department of Medicine, University of Mississippi Medical Center, Jackson, MS, USA. License: CC BY 3.0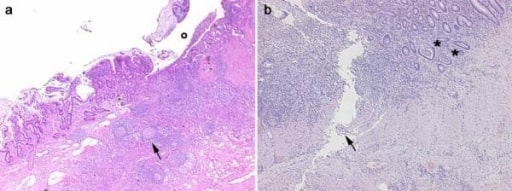
Histological images obtained from 2 inflammatory bowel disease patients. Panel a, CD: in the transmural section is clearly evident an ulceration (o) in the mucosa and submucosa with diffuse inflammatory infiltrations, pseudo-follicle nodules (arrow), and fibrosis of the intestinal wall. Panel b, UC: the inflammatory infiltration is more evident in the mucosa and submucosa with crypt abscesses (asterisks). A serpiginous linear ulcer is evident (arrow).
Image: “Histological images obtained from two IBD patients enrolled in the study affected by CD” by Department of Surgery, Ospedale Maggiore di Milano, IRCCS, University of Milan, V. F. Sforza, 35 – 20122, Milan, Italy. License: CC BY 2.0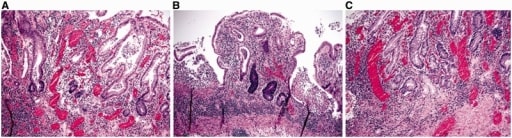
Microscopic features of ulcerative colitis.
A and B: architectural distortion, including shortening of crypts, variation in the sizes and shapes of crypts, and basal lymphoplasmacytosis (A & B: H&E stain; 100X).
C: Paneth cell metaplasia and pyloric gland metaplasia in the left colon (H&E stain; 100X).
Medical therapies for UC depend on the severity of the disease. The 2 main therapeutic goals are:
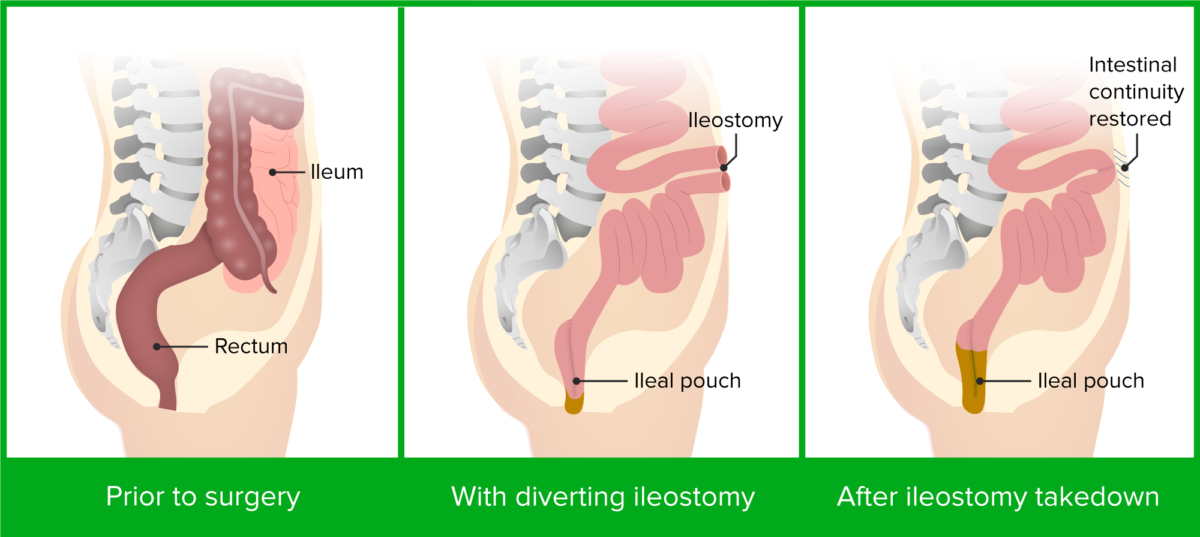
Colectomy and ileal pouch-anal anastomosis
Image by Lecturio.The following conditions are differential diagnoses for ulcerative colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis:
| Crohn’s disease | Ulcerative colitis Colitis Inflammation of the colon section of the large intestine, usually with symptoms such as diarrhea (often with blood and mucus), abdominal pain, and fever. Pseudomembranous Colitis | |
|---|---|---|
| Pattern of involvement |
Skip lesions
Skip lesions
Crohn Disease in any part of the GI tract:
|
Continuous lesions:
|
| GI symptoms | Usually non-bloody diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, may be bloody at times |
Bloody diarrhea
Bloody diarrhea
Diarrhea
|
| Extraintestinal manifestations | Cholelithiasis Cholelithiasis Cholelithiasis (gallstones) is the presence of stones in the gallbladder. Most gallstones are cholesterol stones, while the rest are composed of bilirubin (pigment stones) and other mixed components. Patients are commonly asymptomatic but may present with biliary colic (intermittent pain in the right upper quadrant). Cholelithiasis and nephrolithiasis Nephrolithiasis Nephrolithiasis is the formation of a stone, or calculus, anywhere along the urinary tract caused by precipitations of solutes in the urine. The most common type of kidney stone is the calcium oxalate stone, but other types include calcium phosphate, struvite (ammonium magnesium phosphate), uric acid, and cystine stones. Nephrolithiasis with calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes oxalate stones | Primary sclerosing cholangitis Primary Sclerosing Cholangitis Primary sclerosing cholangitis (PSC) is an inflammatory disease that causes fibrosis and strictures of the bile ducts. The exact etiology is unknown, but there is a strong association with IBD. Patients typically present with an insidious onset of fatigue, pruritus, and jaundice, which can progress to cirrhosis and complications related to biliary obstruction. Primary Sclerosing Cholangitis |
|
||
| Complications |
|
|
|
||
| Macroscopic findings |
Transmural inflammation
Transmural inflammation
Crohn Disease
|
Mucosal and submucosal
inflammation
Inflammation
Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function.
Inflammation
|
| Microscopic findings |
|
|
| Treatment |
|
|