Transfusion-related complications occur during or after a blood product is given. These complications can be classified as immunologic or non-immunologic, and as acute or delayed. Non-immunologic reactions are caused by the transmission of disease in blood products, and immunologic reactions are antigen-antibody-mediated. Symptoms can range from mild itching, chills Chills The sudden sensation of being cold. It may be accompanied by shivering. Fever, and urticaria Urticaria Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives) ( hives Hives Urticaria is raised, well-circumscribed areas (wheals) of edema (swelling) and erythema (redness) involving the dermis and epidermis with associated pruritus (itch). Urticaria is not a single disease but rather is a reaction pattern representing cutaneous mast cell degranulation. Urticaria (Hives)) to high fever Fever Fever is defined as a measured body temperature of at least 38°C (100.4°F). Fever is caused by circulating endogenous and/or exogenous pyrogens that increase levels of prostaglandin E2 in the hypothalamus. Fever is commonly associated with chills, rigors, sweating, and flushing of the skin. Fever, severe shortness of breath Shortness of breath Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, jaundice Jaundice Jaundice is the abnormal yellowing of the skin and/or sclera caused by the accumulation of bilirubin. Hyperbilirubinemia is caused by either an increase in bilirubin production or a decrease in the hepatic uptake, conjugation, or excretion of bilirubin. Jaundice, hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension, or hemoglobinuria. Severe reactions can lead to death.
Last updated: Dec 15, 2025
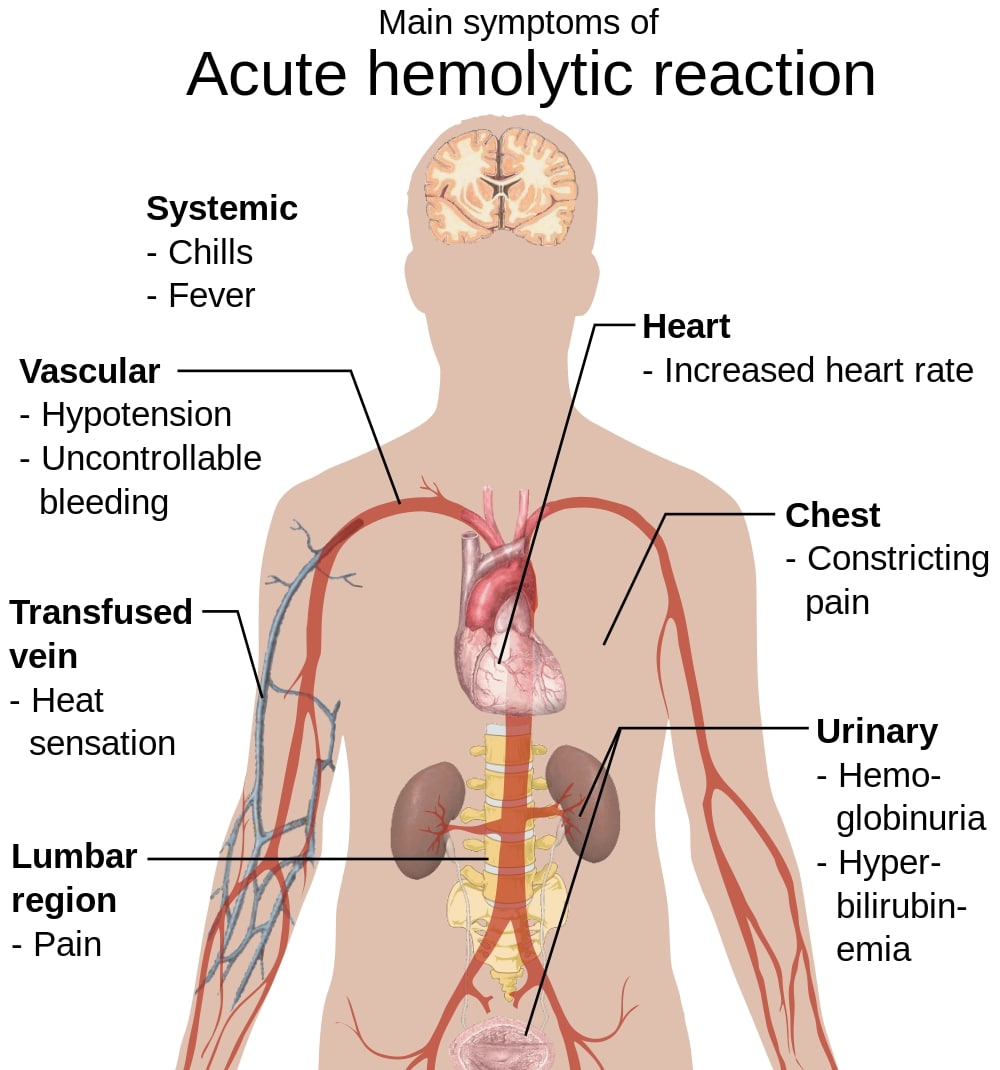
Signs and symptoms of acute hemolytic transfusion reactions
Image: “Main symptoms of acute hemolytic reaction” by Mikael Häggström. License: Public Domain, edited by Lecturio.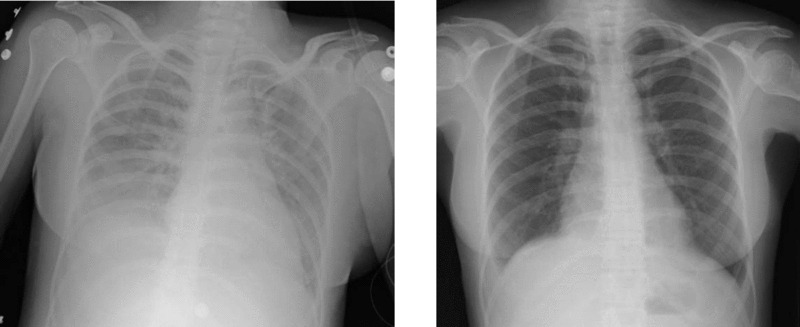
Chest X-ray of TRALI showing bilateral diffuse infiltrates (left); chest X-ray of the same subject after treatment (right)
Image: “Two chest X-rays” by Altaf Gauhar Haji et al. License: CC BY 2.0, edited by Lecturio.