Thrombolytics, also known as fibrinolytics, include recombinant tissue plasminogen activator Tissue plasminogen activator A proteolytic enzyme in the serine protease family found in many tissues which converts plasminogen to fibrinolysin. It has fibrin-binding activity and is immunologically different from urokinase-type plasminogen activator. The primary sequence, composed of 527 amino acids, is identical in both the naturally occurring and synthetic proteases. Hemostasis ( tPA tPA Ischemic Stroke) (i.e., alteplase, reteplase, and tenecteplase), urokinase, and streptokinase. The agents promote the breakdown of a blood clot by converting plasminogen Plasminogen Precursor of plasmin (fibrinolysin). It is a single-chain beta-globulin of molecular weight 80-90, 000 found mostly in association with fibrinogen in plasma; plasminogen activators change it to fibrinolysin. It is used in wound debriding and has been investigated as a thrombolytic agent. Hemostasis to plasmin Plasmin A product of the lysis of plasminogen (profibrinolysin) by plasminogen activators. It is composed of two polypeptide chains, light (b) and heavy (a), with a molecular weight of 75, 000. It is the major proteolytic enzyme involved in blood clot retraction or the lysis of fibrin and quickly inactivated by antiplasmins. Hemostasis, which then degrades fibrin Fibrin A protein derived from fibrinogen in the presence of thrombin, which forms part of the blood clot. Rapidly Progressive Glomerulonephritis. Thrombolytics are particularly helpful for conditions related to vascular obstruction by a blood clot (e.g., acute STEMI, pulmonary embolism Pulmonary Embolism Pulmonary embolism (PE) is a potentially fatal condition that occurs as a result of intraluminal obstruction of the main pulmonary artery or its branches. The causative factors include thrombi, air, amniotic fluid, and fat. In PE, gas exchange is impaired due to the decreased return of deoxygenated blood to the lungs. Pulmonary Embolism (PE), deep venous thrombosis Venous thrombosis The formation or presence of a blood clot (thrombus) within a vein. Budd-Chiari Syndrome ( DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis), and acute ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke). Efficacy declines the longer tissue ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage persists; therefore, timing of therapy is particularly important in myocardial infarction Myocardial infarction MI is ischemia and death of an area of myocardial tissue due to insufficient blood flow and oxygenation, usually from thrombus formation on a ruptured atherosclerotic plaque in the epicardial arteries. Clinical presentation is most commonly with chest pain, but women and patients with diabetes may have atypical symptoms. Myocardial Infarction and stroke. Life-threatening bleeding and allergic reactions Allergic Reactions Type I hypersensitivity reaction against plasma proteins in donor blood Transfusion Reactions are potentially serious complications. Weighing the risks and benefits of thrombolytics and evaluating individuals for contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation/bleeding risk before initiating therapy is important.
Last updated: Dec 15, 2025
Normal physiology:
Thrombolytics (also known as fibrinolytics):
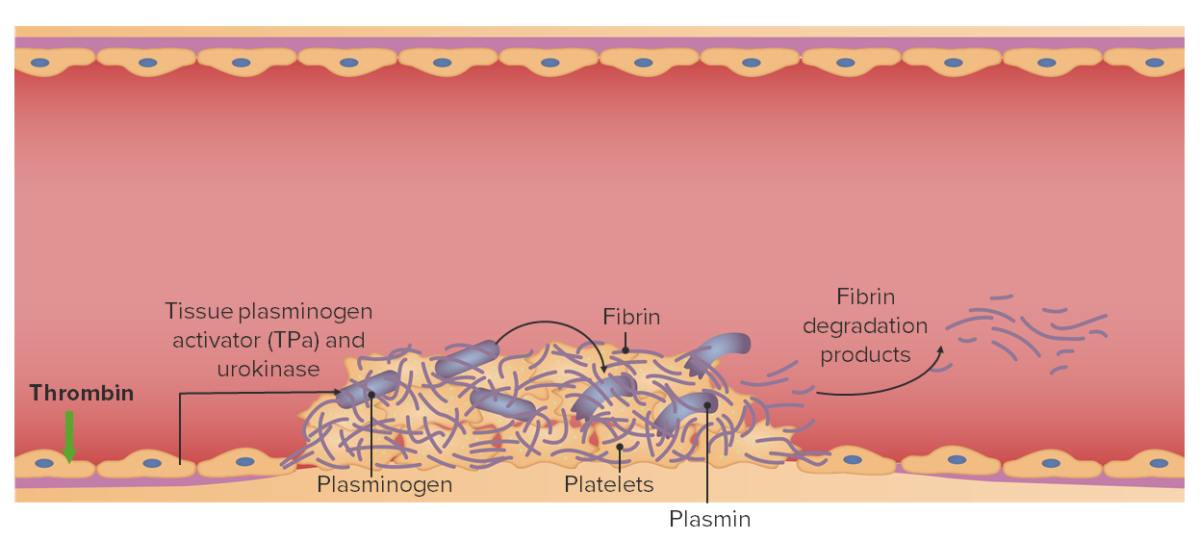
Normal physiology relating to thrombolysis:
Endogenous tissue plasminogen activator (TPa) and urokinase cleave plasminogen into plasmin, resulting in the degradation of fibrin.
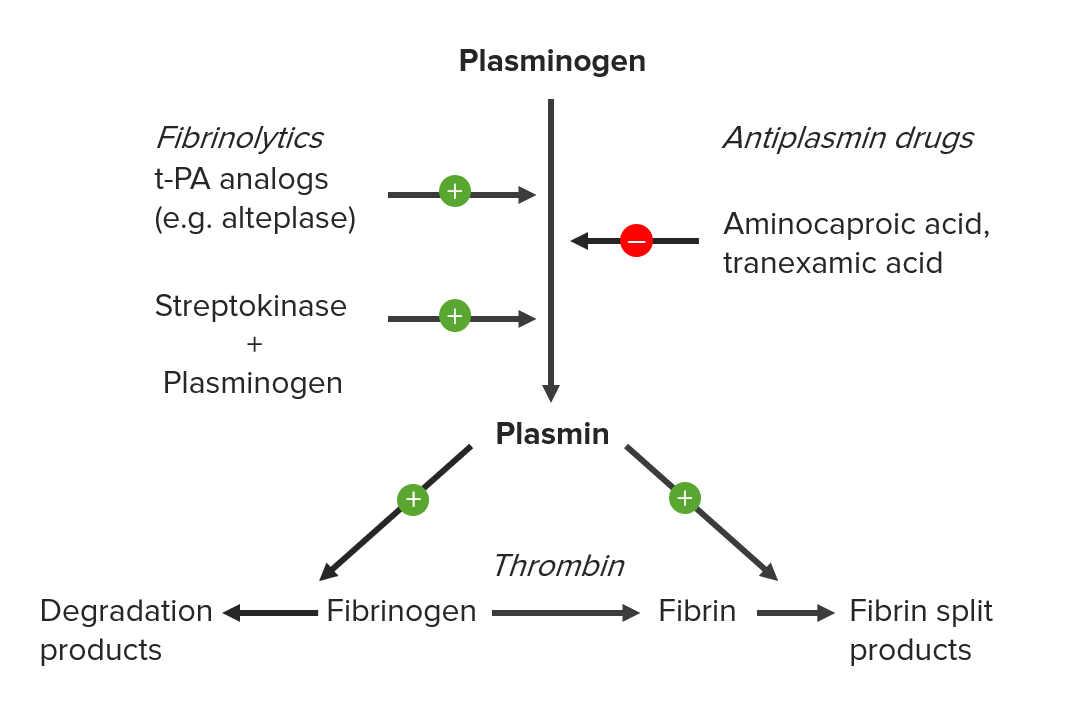
Mechanism of action of thrombolytic (fibrinolytic) agents:
The agents act by converting plasminogen to plasmin, which can then break down fibrin. Streptokinase must 1st form a complex with plasminogen to cleave plasminogen.
ST elevation myocardial infarction ST elevation myocardial infarction A clinical syndrome defined by myocardial ischemia symptoms; persistent elevation in the ST segments of the electrocardiogram; and release of biomarkers of myocardial necrosis (e.g., elevated troponin levels). ST segment elevation in the ECG is often used in determining the treatment protocol. Myocardial Infarction (STEMI):
Acute ischemic stroke Ischemic Stroke An ischemic stroke (also known as cerebrovascular accident) is an acute neurologic injury that occurs as a result of brain ischemia; this condition may be due to cerebral blood vessel occlusion by thrombosis or embolism, or rarely due to systemic hypoperfusion. Ischemic Stroke:
Pulmonary embolism Pulmonary Embolism Pulmonary embolism (PE) is a potentially fatal condition that occurs as a result of intraluminal obstruction of the main pulmonary artery or its branches. The causative factors include thrombi, air, amniotic fluid, and fat. In PE, gas exchange is impaired due to the decreased return of deoxygenated blood to the lungs. Pulmonary Embolism (PE):
Deep vein thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus ( DVT DVT Deep vein thrombosis (DVT) usually occurs in the deep veins of the lower extremities. The affected veins include the femoral, popliteal, iliofemoral, and pelvic veins. Proximal DVT is more likely to cause a pulmonary embolism (PE) and is generally considered more serious. Deep Vein Thrombosis):
Additional indications:
Use thrombolytics cautiously. The medications have a significant risk of bleeding, which can be life threatening or fatal.
Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation depend on the medication, dosing, and pathology and may include:
An increased risk of bleeding may occur in individuals taking: