Thoracic aortic aneurysm (TAA) is the abnormal dilation of a segment of the thoracic aorta, usually the ascending aorta. Most TAAs are due to degenerative aortic disorders, commonly in patients > 65 years of age. Genetic TAAs account for 20% of cases and are frequently found in younger patients. Most TAAs are asymptomatic (incidentally found in imaging) but could present with symptoms from their effects on surrounding structures. Aortic rupture is a life-threatening emergency. Among diagnostic imaging studies, computed tomography (CT) angiography is the most widely utilized. In asymptomatic cases, aortic expansion is monitored. Operative repair is recommended for symptomatic TAAs and increasing aortic diameter (criteria varies with location and underlying condition).
Last updated: Sep 12, 2025
Thoracic aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms ( TAA TAA Thoracic aortic aneurysm (TAA) is the abnormal dilation of a segment of the thoracic aorta, usually the ascending aorta. Most TAAs are due to degenerative aortic disorders, commonly in patients > 65 years of age. Most TAAs are asymptomatic (incidentally found in imaging) but could present with symptoms from its effects on surrounding structures. Thoracic Aortic Aneurysms):
Types:
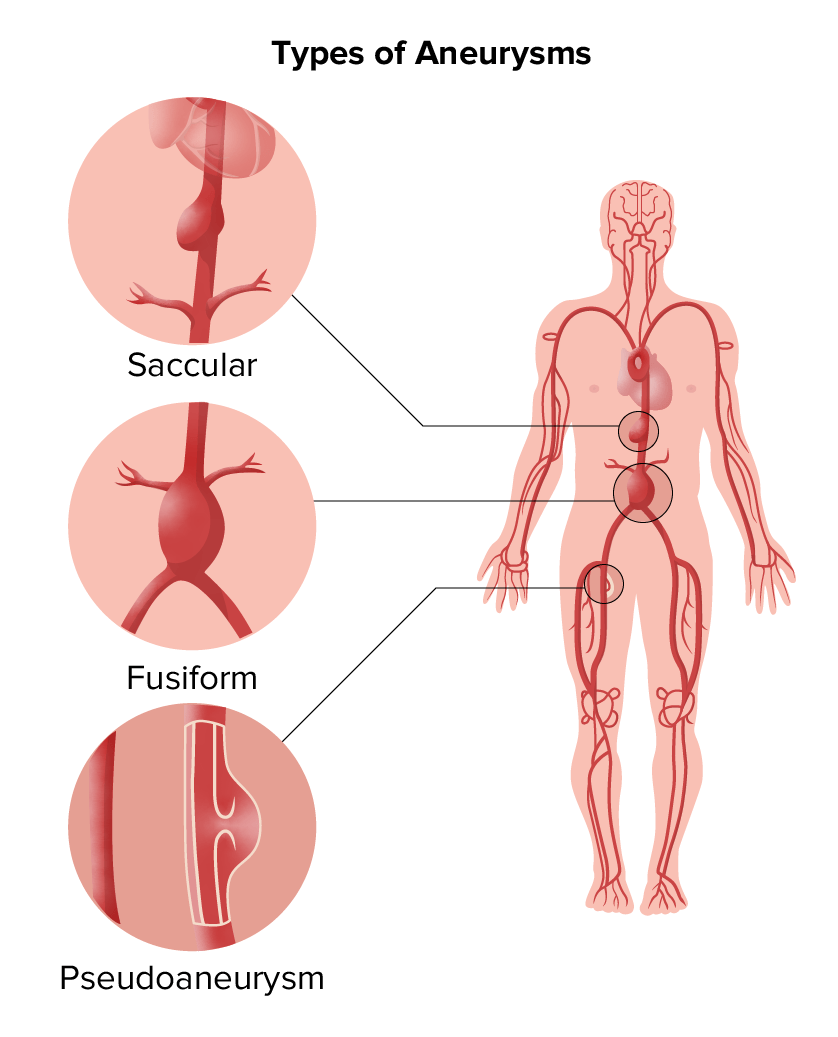
Types of aneurysms:
Saccular and fusiform aneurysms are in the category of true aneurysms; pseudoaneurysm is another type.
Location:
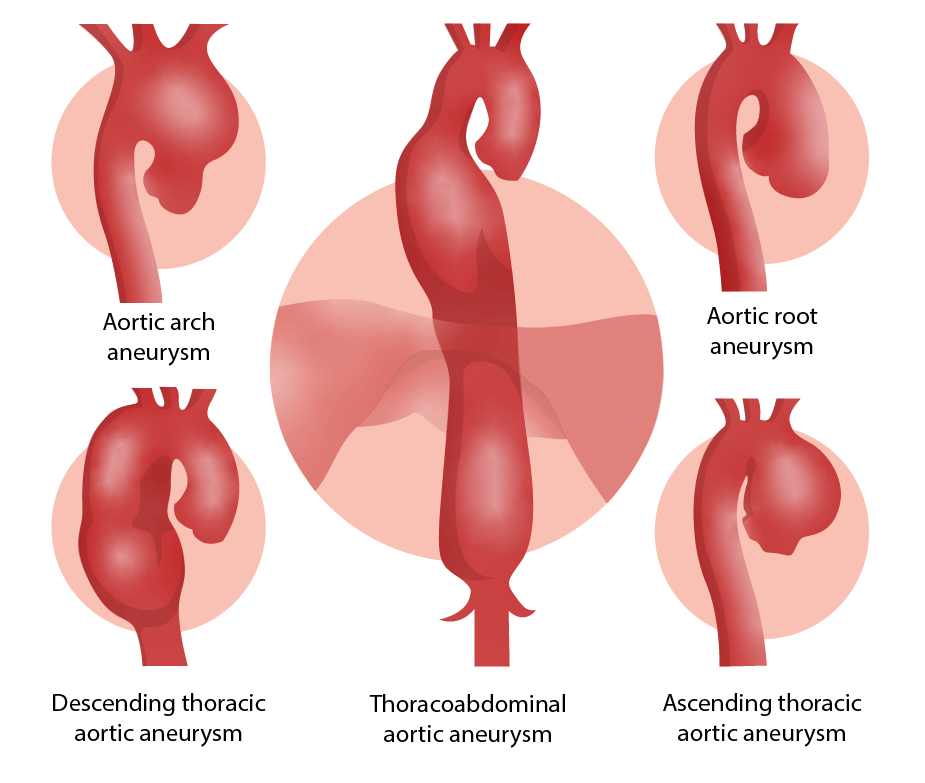
Locations of aortic aneurysms
Image by Lecturio.Management may vary based on practice location. The following information is based on US and European guidelines.
| Management of asymptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship | Degenerative ascending or aortic root aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms | Descending aortic aneurysm Descending aortic aneurysm Thoracic Aortic Aneurysms |
|---|---|---|
|
Annual
CTA
CTA
A non-invasive method that uses a ct scanner for capturing images of blood vessels and tissues. A contrast material is injected, which helps produce detailed images that aid in diagnosing vascular diseases.
Pulmonary Function Tests/
MRA
MRA
Imaging of the Heart and Great Vessels
( echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) to follow valvular disease if needed) |
4–4.4 cm | 4–4.9 cm |
| Biannual (every 6 months)
CTA
CTA
A non-invasive method that uses a ct scanner for capturing images of blood vessels and tissues. A contrast material is injected, which helps produce detailed images that aid in diagnosing vascular diseases.
Pulmonary Function Tests/
MRA
MRA
Imaging of the Heart and Great Vessels
( echocardiography Echocardiography Ultrasonic recording of the size, motion, and composition of the heart and surrounding tissues. The standard approach is transthoracic. Tricuspid Valve Atresia (TVA) to follow valvular disease if needed) |
4.5–5.4 cm or rapid expansion | 5–6 cm |
| Consider elective repair |
≥ 5.5 cm
Rapid expansion (> 0.5 cm/year) ≥ 4.5 cm if aortic valve Aortic valve The valve between the left ventricle and the ascending aorta which prevents backflow into the left ventricle. Heart: Anatomy surgery or coronary bypass needed |
≥ 5.5 cm, consider thoracic endovascular repair (TEVAR);
≥ 6 cm (TEVAR not technically possible) for open surgery; Rapid expansion (> 0.5 cm/year) |
Indications for operative repair:[3,5,11]
Preparation for emergency surgery:[12–15]
| Class I | Class II | Class III | Class IV | |
|---|---|---|---|---|
| Percentage of blood loss | < 15 | 15–30 | 30–40 | > 40 |
| Pulse rate | Normal | 100–120 | 120–140 | > 140 |
| Blood pressure | Normal | Normal | Decreased | Significantly decreased |
| Pulse pressure | Normal | Decreased | Decreased | Decreased |
| Respiratory rate Respiratory rate The number of times an organism breathes with the lungs (respiration) per unit time, usually per minute. Pulmonary Examination | 14–20 | 20–30 | 30–40 | > 35 |
| Mental status | Slightly anxious | Mildly anxious | Anxious, confused | Confused, lethargic |
| Urine output (mL/hr) | > 30 | 20–30 | 5–15 | Minimal |
| Fluid resuscitation Resuscitation The restoration to life or consciousness of one apparently dead. . Neonatal Respiratory Distress Syndrome strategy | Crystalloid Crystalloid Isotonic solutions of mineral salts, such as ringer’s lactate and sodium chloride (saline solution), used in fluid therapy to rehydrate blood volume. Intravenous Fluids | Crystalloid Crystalloid Isotonic solutions of mineral salts, such as ringer’s lactate and sodium chloride (saline solution), used in fluid therapy to rehydrate blood volume. Intravenous Fluids, possibly blood products | Type-specific blood | Massive transfusion protocol |
Operative options:[3,5,12,13]
Differential diagnoses of TAA TAA Thoracic aortic aneurysm (TAA) is the abnormal dilation of a segment of the thoracic aorta, usually the ascending aorta. Most TAAs are due to degenerative aortic disorders, commonly in patients > 65 years of age. Most TAAs are asymptomatic (incidentally found in imaging) but could present with symptoms from its effects on surrounding structures. Thoracic Aortic Aneurysms include the following conditions:
Diagnosis Codes:
These codes are used to classify a thoracic
aortic aneurysm
Aortic aneurysm
An abnormal balloon- or sac-like dilatation in the wall of aorta.
Thoracic Aortic Aneurysms based on its status, distinguishing between an unruptured
aneurysm
Aneurysm
An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening.
Thoracic Aortic Aneurysms and a life-threatening ruptured
aneurysm
Aneurysm
An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening.
Thoracic Aortic Aneurysms.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | I71.2 | Thoracic aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms, without rupture |
| ICD-10-CM | I71.1 | Thoracic aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms, ruptured |
Evaluation & Workup:
This CPT code is for a CT
angiography
Angiography
Radiography of blood vessels after injection of a contrast medium.
Cardiac Surgery of the chest, the primary imaging modality for diagnosing, measuring, and monitoring thoracic aortic aneurysms and for planning surgical repair.
| Coding System | Code | Description |
|---|---|---|
| CPT | 71275 | Computed tomography angiography Angiography Radiography of blood vessels after injection of a contrast medium. Cardiac Surgery, chest (noncoronary), with contrast material(s) |
Procedures/Interventions:
These codes represent the surgical options for repair. TEVAR is a minimally invasive endovascular approach, while an open repair involves a
thoracotomy
Thoracotomy
Surgical incision into the chest wall.
Thoracic Surgery and
graft
Graft
A piece of living tissue that is surgically transplanted
Organ Transplantation placement.
| Coding System | Code | Description |
|---|---|---|
| CPT | 33880 | Endovascular repair of descending thoracic aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy (eg, aneurysm Aneurysm An aneurysm is a bulging, weakened area of a blood vessel that causes an abnormal widening of its diameter > 1.5 times the size of the native vessel. Aneurysms occur more often in arteries than in veins and are at risk of dissection and rupture, which can be life-threatening. Thoracic Aortic Aneurysms, pseudoaneurysm Pseudoaneurysm Not an aneurysm but a well-defined collection of blood and connective tissue outside the wall of a blood vessel or the heart. It is the containment of a ruptured blood vessel or heart, such as sealing a rupture of the left ventricle. False aneurysm is formed by organized thrombus and hematoma in surrounding tissue. Thoracic Aortic Aneurysms, dissection, penetrating ulcer, intramural hematoma Intramural hematoma Dissection of the Carotid and Vertebral Arteries, or traumatic disruption); involving coverage of left subclavian artery origin |
| CPT | 33875 | Descending thoracic aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy graft Graft A piece of living tissue that is surgically transplanted Organ Transplantation, with or without bypass |