Tardive dyskinesia (TD) is a serious, potentially irreversible neurologic movement disorder that can potentially be caused by any dopamine receptor-blocking agent. The most commonly implicated drugs are antipsychotics and metoclopramide, an antiemetic drug. TD is characterized by involuntary, repetitive movements, typically resulting from long-term use of the offending agents. These movements include grimacing, tongue protrusion, lip-smacking, and rapid eye blinking, but movements may also occur in the trunk and extremities. Early clinical recognition of TD is important to allow for the discontinuation of the causative drug, if possible, thereby reducing the risk of irreversibility. In addition to stopping the causative drug, other approaches for managing TD involve either switching to an alternative medication, reducing the current drug's dosage, or employing symptomatic treatments in moderate to severe cases. Symptomatic treatments most commonly include the utilization of vesicular monoamine transporter type 2 (VMAT2) inhibitors and botulinum toxin injections. For patients suffering from permanent and debilitating TD, surgical interventions, such as deep brain stimulation, may be considered as a last resort.
Last updated: Dec 15, 2025
Tardive dyskinesia (TD) is a hyperkinetic, medication-induced, involuntary movement disorder.
Causative agents include medications with dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS receptor-blocking mechanisms of action:
The underlying pathophysiology of hyperkinetic movement in TD is not fully understood, but may be related to structural and biochemical disturbances in the basal ganglia Basal Ganglia Basal ganglia are a group of subcortical nuclear agglomerations involved in movement, and are located deep to the cerebral hemispheres. Basal ganglia include the striatum (caudate nucleus and putamen), globus pallidus, substantia nigra, and subthalamic nucleus. Basal Ganglia: Anatomy of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification, which are primarily responsible for motor Motor Neurons which send impulses peripherally to activate muscles or secretory cells. Nervous System: Histology control and require the appropriate release of dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS at their input nuclei for their effective operation:
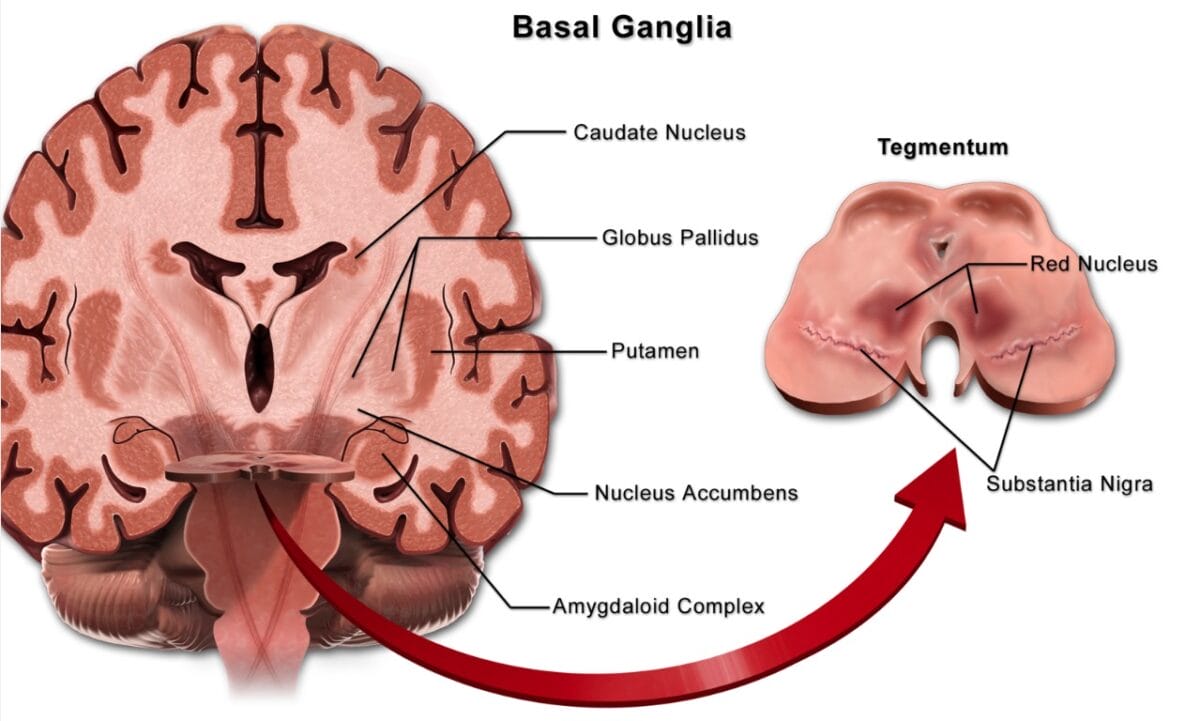
The basal ganglia consist of a group of subcortical nuclei responsible primarily for motor control, as well as other roles such as motor learning, executive functions and behaviors, and emotions. Their proper functioning requires dopamine to be released at the input nuclei. The term “basal ganglia” classically refers to the caudate-putamen (also called the striatum) and the globus pallidus, whereas related nuclei consist of structures located in the subthalamus (the subthalamic nucleus, just above the tegmental area), the midbrain (the substantia nigra), and the pons (the pedunculopontine nucleus).
Image: “Blausen 0076 – Basal ganglia – English labels” by Blausen.com staff (2014). License: CC BY 4.0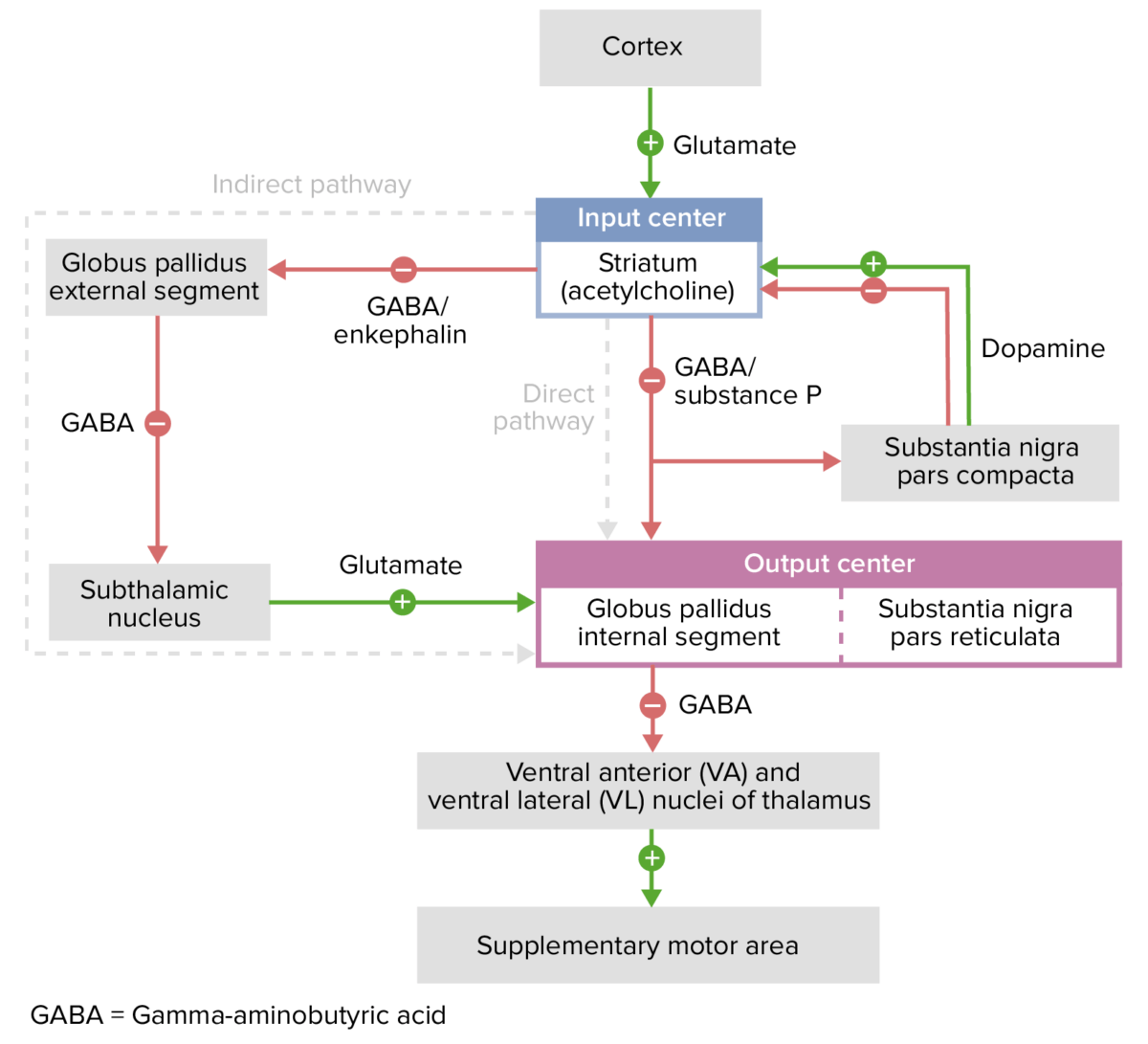
Excitatory and inhibitory pathways of the basal ganglia:
GABA serves as an essential inhibitory neurotransmitter in the basal ganglia, working in concert with dopamine to regulate motor control. The balance of GABAergic inhibition and dopaminergic modulation is critical for the smooth execution of movements.
Dopamine has a dual effect on the neurons of the striatum. It activates the neurons in the direct (D1 receptor) pathway and inhibits those in the indirect (D2 receptor) pathway.
When dopamine levels in the striatum decrease, the indirect pathway becomes hyperactive, while the direct pathway’s activity diminishes. This hyperactivity in the striatal projection to the lateral globus pallidus leads to reduced activity in pallidosubthalamic neurons, which results in increased activity of the subthalamic nucleus. The subthalamic nucleus then excessively stimulates the medial globus pallidus and the substantia nigra pars reticulata. This effect is further intensified by the reduced activity of the inhibitory GABAergic neurons of the direct pathway. As a result, the basal ganglia’s output excessively inhibits the motor thalamus and its excitatory connections to the cerebral cortex.
In individuals with tardive dyskinesia (TD), chronic use of dopamine-blocking medications, such as antipsychotics, can disrupt the normal balance of dopamine signaling in the basal ganglia. This disruption can result in an imbalance between the indirect and direct pathways, leading to abnormal output to the cerebral cortex. This imbalance can cause abnormal involuntary movements, which are the hallmark of TD.
The clinical presentation of TD is variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables, and can involve different body regions and types of involuntary movements. Symptoms may be insidious in onset, particularly with tongue Tongue The tongue, on the other hand, is a complex muscular structure that permits tasting and facilitates the process of mastication and communication. The blood supply of the tongue originates from the external carotid artery, and the innervation is through cranial nerves. Lips and Tongue: Anatomy movements. The repetitive movements characteristic of TD can be either intermittent or continuous, contributing to the complexity of the disorder.
Head (most common):
Trunk:
Extremities:
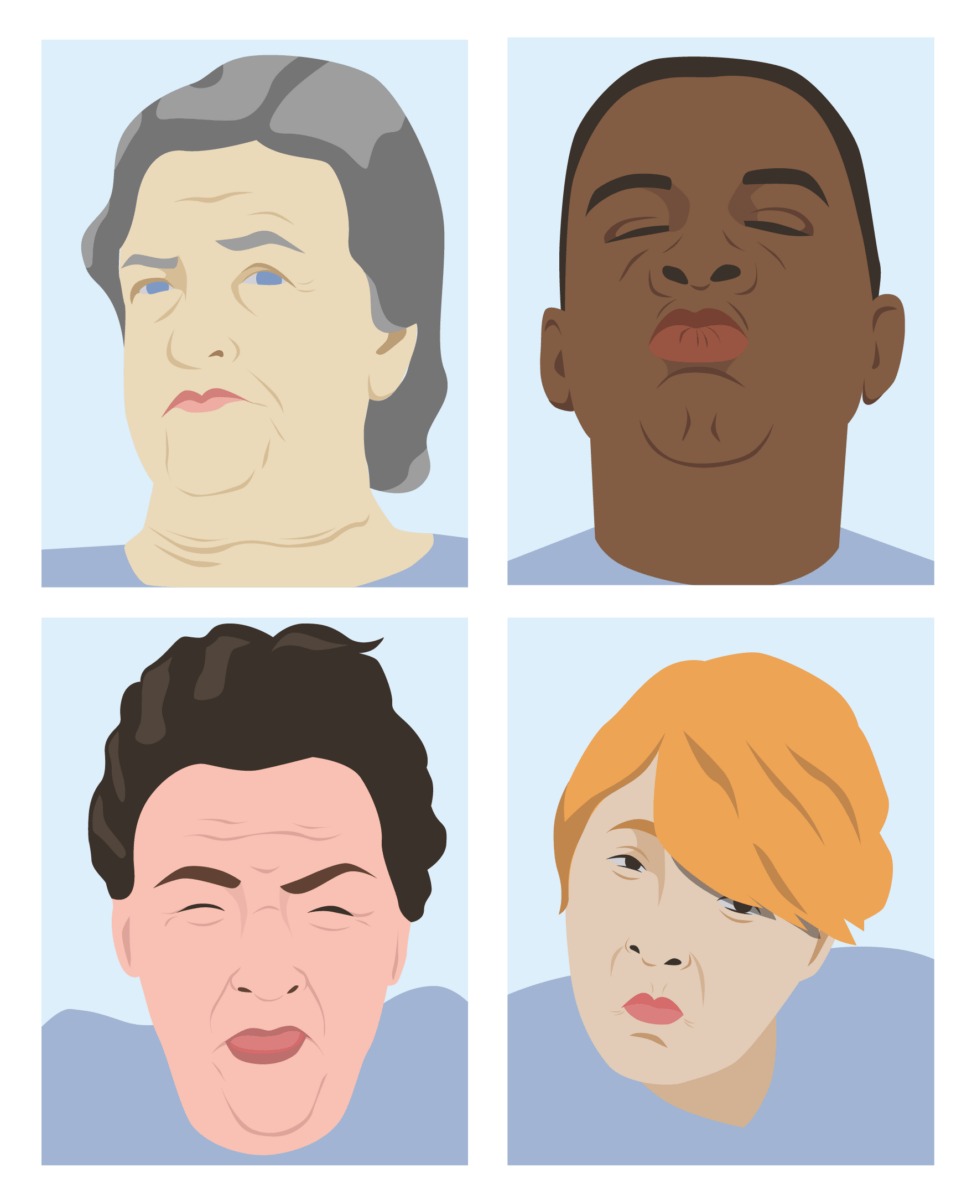
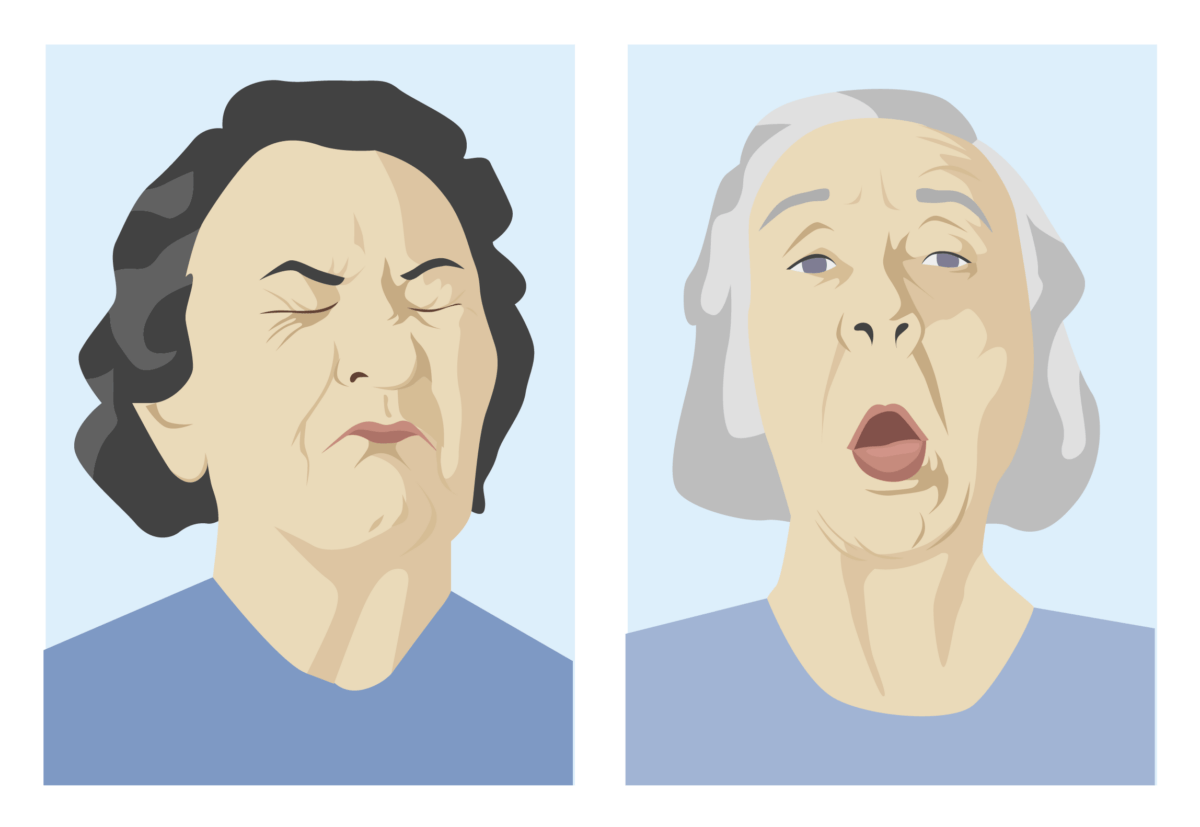
Common facial movements of tardive dyskinesia:
Top left: Facial grimacing
Top right: Lip puckering
Bottom left: Tongue protrusion and excessive blinking
Bottom right: Pursed lips
This is a subtype of TD where dystonic characteristics predominate.
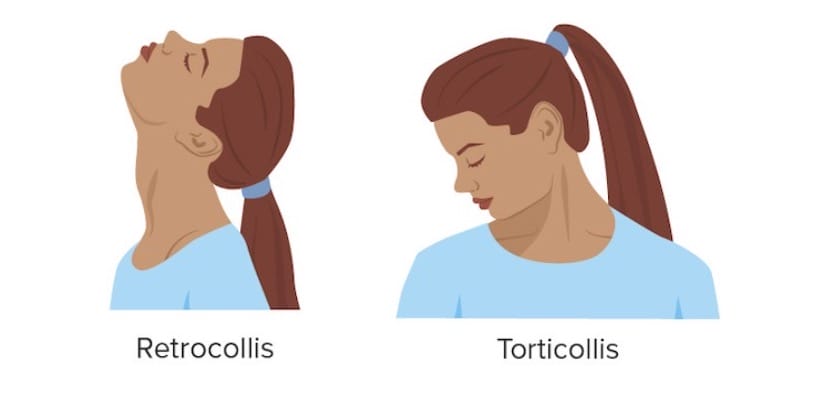
Tardive dystonia:
Torticollis refers to muscle contraction or spasm that forces the head to turn to one side. When this process results in neck extension, it is referred to as retrocollis.
Tardive dystonia:
The image on the left shows eyelid spasms (blepharospasm), spasm of jaw closure (jaw dystonia), and mouth pursing. The image on the right shows spasm of jaw opening and mouth retraction.
The diagnosis of TD is clinical and should be suspected if:
A physical examination should be performed to evaluate for signs of an alternative diagnosis.
Testing is not necessary for the diagnosis of TD, but may be useful to rule out other causes of the patient’s symptoms, particularly if the diagnosis is unclear. An evaluation may include:
There are no curative treatments for TD. Thus, prevention is paramount.
Discontinue the offending medication at the first signs of TD, if possible:
Medical therapy:
Other therapies:
| Disorder | Etiology | Typical onset of symptoms (after drug initiation) | Clinical presentation | Management |
|---|---|---|---|---|
| Akathisia |
Dopamine
Dopamine
One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement.
Receptors and Neurotransmitters of the CNS antagonists:
|
Within days | Inner restlessness (inability to stay still):
|
Reduce or discontinue offending medication
Symptom management:
|
| Drug-induced dystonia Dystonia Dystonia is a hyperkinetic movement disorder characterized by the involuntary contraction of muscles, resulting in abnormal postures or twisting and repetitive movements. Dystonia can present in various ways as may affect many different skeletal muscle groups. Dystonia | Within days | Involuntary contraction of major muscle groups, such as:
|
Discontinue offending medication
Symptom management:
|
|
| Parkinsonism Parkinsonism West Nile Virus | Within a month |
|
Reduce or discontinue offending medication
Symptom management:
|
Tardive dyskinesia | Chronic use of dopamine Dopamine One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement. Receptors and Neurotransmitters of the CNS antagonists | After 3 months | Involuntary movements, such as:
|
Discontinue offending medication
Symptom management: VMAT2 inhibitors |
Neuroleptic malignant syndrome Neuroleptic malignant syndrome Neuroleptic malignant syndrome (NMS) is a rare, idiosyncratic, and potentially life-threatening reaction to antipsychotic drugs. Neuroleptic malignant syndrome presents with ≥ 2 of the following cardinal symptoms: fever, altered mental status, muscle rigidity, and autonomic dysfunction. Neuroleptic Malignant Syndrome |
Dopamine
Dopamine
One of the catecholamine neurotransmitters in the brain. It is derived from tyrosine and is the precursor to norepinephrine and epinephrine. Dopamine is a major transmitter in the extrapyramidal system of the brain, and important in regulating movement.
Receptors and Neurotransmitters of the CNS antagonists
Withdrawal of dopaminergic agents (e.g., levodopa Levodopa The naturally occurring form of dihydroxyphenylalanine and the immediate precursor of dopamine. Unlike dopamine itself, it can be taken orally and crosses the blood-brain barrier. It is rapidly taken up by dopaminergic neurons and converted to dopamine. It is used for the treatment of parkinsonian disorders and is usually given with agents that inhibit its conversion to dopamine outside of the central nervous system. Parkinson’s Disease Drugs) |
Hours to days |
Altered mental status
Altered Mental Status
Sepsis in Children
Autonomic dysregulation Autonomic Dysregulation Neuroleptic Malignant Syndrome:
Severe muscular rigidity Severe muscular rigidity Neuroleptic Malignant Syndrome |
Discontinue offending medication
Symptom management:
|
Serotonin Serotonin A biochemical messenger and regulator, synthesized from the essential amino acid l-tryptophan. In humans it is found primarily in the central nervous system, gastrointestinal tract, and blood platelets. Serotonin mediates several important physiological functions including neurotransmission, gastrointestinal motility, hemostasis, and cardiovascular integrity. Receptors and Neurotransmitters of the CNS syndrome | Serotonergic medications:
|
Within a day |
Altered mental status
Altered Mental Status
Sepsis in Children
Autonomic dysregulation Autonomic Dysregulation Neuroleptic Malignant Syndrome:
Neuromuscular hyperactivity Hyperactivity Attention Deficit Hyperactivity Disorder:
GI stimulaton:
|
Discontinue offending medication
Symptom management:
|