Short bowel syndrome is a malabsorptive condition most commonly associated with extensive intestinal resection for etiologies such as Crohn's disease, bowel obstruction Bowel obstruction Any impairment, arrest, or reversal of the normal flow of intestinal contents toward the anal canal. Ascaris/Ascariasis, trauma, radiation Radiation Emission or propagation of acoustic waves (sound), electromagnetic energy waves (such as light; radio waves; gamma rays; or x-rays), or a stream of subatomic particles (such as electrons; neutrons; protons; or alpha particles). Osteosarcoma therapy, and vascular insufficiency Vascular insufficiency Anal Fissure. The short length of bowel results in insufficient surface area for fluid and electrolyte absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea, electrolyte abnormalities, and dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration. Management options include antimotility agents, antisecretory agents, and total parenteral nutrition Parenteral nutrition The administering of nutrients for assimilation and utilization by a patient who cannot maintain adequate nutrition by enteral feeding alone. Nutrients are administered by a route other than the alimentary canal (e.g., intravenously, subcutaneously). Central Venous Catheter for patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship who cannot maintain themselves with oral intake. Last-resort options include surgical intestinal lengthening procedures and small bowel Small bowel The small intestine is the longest part of the GI tract, extending from the pyloric orifice of the stomach to the ileocecal junction. The small intestine is the major organ responsible for chemical digestion and absorption of nutrients. It is divided into 3 segments: the duodenum, the jejunum, and the ileum. Small Intestine: Anatomy transplant.
Last updated: Dec 15, 2025
Several factors determine the degree of intestinal function loss after bowel resection:
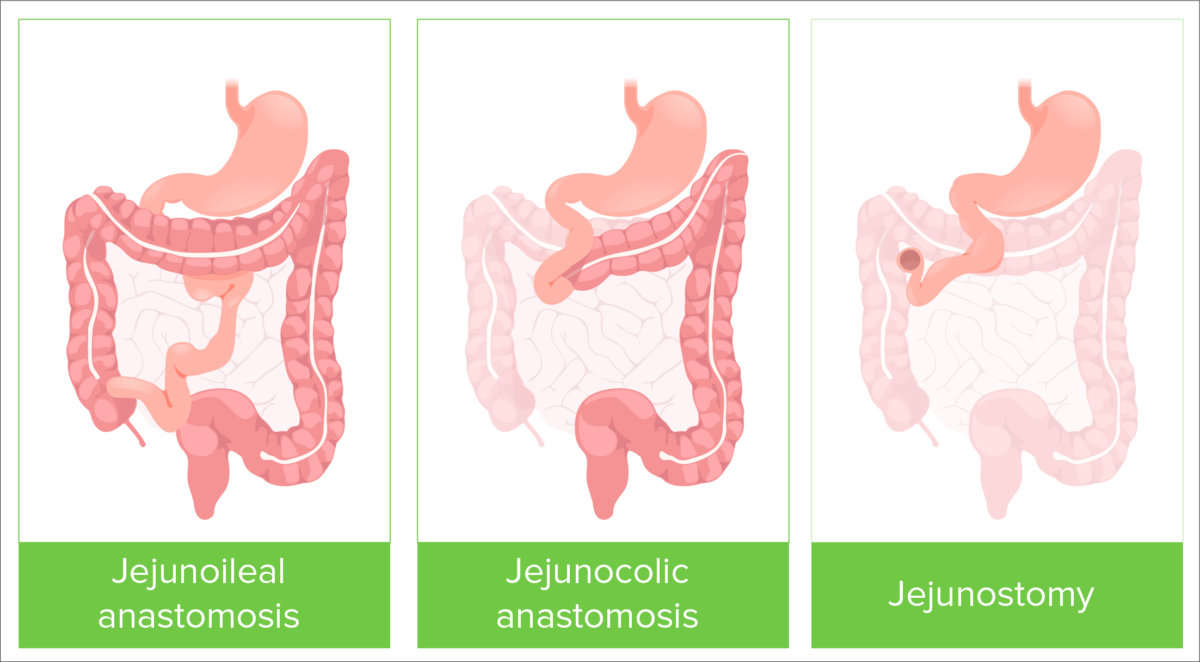
Types of bowel resection
Image by Lecturio.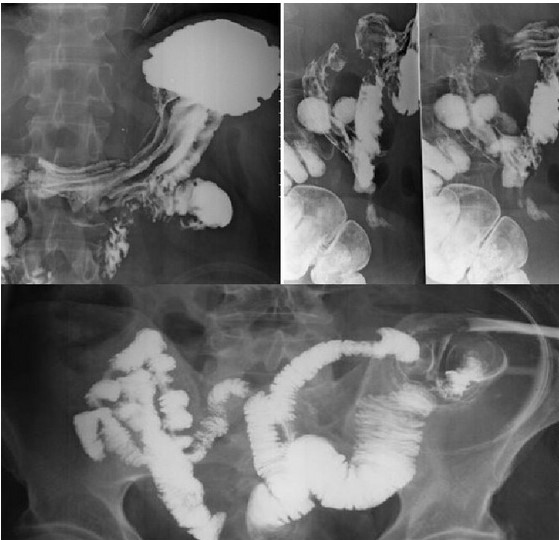
Radiological examinations demonstrating short bowel syndrome
Image: “Colectomy and acute renal failure: a case report with unusual presentation” by Sahin OZ, Bilir C, Ayaz T. License: CC BY 3.0, edited by Lecturio.Acute phase:
Adaptation phase:
Maintenance phase:
The following table summarizes possible laboratory findings in SBS that correlate with signs and symptoms of malabsorption Malabsorption General term for a group of malnutrition syndromes caused by failure of normal intestinal absorption of nutrients. Malabsorption and Maldigestion.
| Manifestation | Laboratory findings |
|---|---|
| Steatorrhea Steatorrhea A condition that is characterized by chronic fatty diarrhea, a result of abnormal digestion and/or intestinal absorption of fats. Diarrhea | ↑ Fecal fat content |
| Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea | ↑ Stool osmolality Osmolality Plasma osmolality refers to the combined concentration of all solutes in the blood. Renal Sodium and Water Regulation |
| Bleeding, ecchymosis Ecchymosis Extravasation of blood into the skin, resulting in a nonelevated, rounded or irregular, blue or purplish patch, larger than a petechia. Orbital Fractures | ↑ PT/INR and aPTT |
| Microcytic anemia Microcytic anemia Conditions in which there is a generalized increase in the iron stores of body tissues, particularly of liver and the mononuclear phagocyte system, without demonstrable tissue damage. The name refers to the presence of stainable iron in the tissue in the form of hemosiderin. Anemia: Overview and Types | ↓ Ferritin Ferritin Iron-containing proteins that are widely distributed in animals, plants, and microorganisms. Their major function is to store iron in a nontoxic bioavailable form. Each ferritin molecule consists of ferric iron in a hollow protein shell (apoferritins) made of 24 subunits of various sequences depending on the species and tissue types. Hereditary Hemochromatosis and iron Iron A metallic element with atomic symbol fe, atomic number 26, and atomic weight 55. 85. It is an essential constituent of hemoglobins; cytochromes; and iron-binding proteins. It plays a role in cellular redox reactions and in the transport of oxygen. Trace Elements |
| Macrocytic anemia Macrocytic anemia Anemia characterized by larger than normal erythrocytes, increased mean corpuscular volume (MCV) and increased mean corpuscular hemoglobin (mMCH). Anemia: Overview and Types | ↓ Vitamin B12 and folic acid |
| Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, fractures | ↓ Calcium Calcium A basic element found in nearly all tissues. It is a member of the alkaline earth family of metals with the atomic symbol ca, atomic number 20, and atomic weight 40. Calcium is the most abundant mineral in the body and combines with phosphorus to form calcium phosphate in the bones and teeth. It is essential for the normal functioning of nerves and muscles and plays a role in blood coagulation (as factor IV) and in many enzymatic processes. Electrolytes and vitamin D Vitamin D A vitamin that includes both cholecalciferols and ergocalciferols, which have the common effect of preventing or curing rickets in animals. It can also be viewed as a hormone since it can be formed in skin by action of ultraviolet rays upon the precursors, 7-dehydrocholesterol and ergosterol, and acts on vitamin D receptors to regulate calcium in opposition to parathyroid hormone. Fat-soluble Vitamins and their Deficiencies |
| Lactose intolerance Lactose intolerance Lactose intolerance (LI) describes a constellation of symptoms due to lactase deficiency (LD), the enzyme located in the brush border of the absorptive cells in the small intestine. Lactose is the disaccharide present in milk and requires hydrolysis by lactase to break it down into its 2 absorbable constituents, glucose and galactose. Lactose intolerance typically presents with bloating, abdominal cramping, diarrhea, and flatulence. Lactose Intolerance | Abnormal lactose tolerance Tolerance Pharmacokinetics and Pharmacodynamics test |
| Edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema | ↓ Serum albumin Albumin Serum albumin from humans. It is an essential carrier of both endogenous substances, such as fatty acids and bilirubin, and of xenobiotics in the blood. Liver Function Tests and prealbumin |
Intestinal lengthening procedures:
Transplant: