Septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis is an infection of the joint due to direct inoculation, contiguous extension Extension Examination of the Upper Limbs, or hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases spread of infectious organisms into the joint space. This process causes an acute, inflammatory, monoarticular arthritis Monoarticular Arthritis Septic Arthritis. A variety of organisms have been implicated, most commonly Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess. Previously damaged joints (e.g., rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis) are at the highest risk of infection. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with a swollen, warm, and tender joint, most commonly involving the knee. Positive cultures from arthrocentesis Arthrocentesis Puncture and aspiration of fluid (e.g., synovial fluid) from a joint cavity. It is used sometimes to irrigate or administer drugs into a joint cavity. Septic Arthritis are diagnostic, with antibiotic therapy tailored to the specific organism. Repeated joint aspiration, or surgical drainage, is required in some cases. If the joint space is infected with a prosthetic in place, debridement Debridement The removal of foreign material and devitalized or contaminated tissue from or adjacent to a traumatic or infected lesion until surrounding healthy tissue is exposed. Stevens-Johnson Syndrome and prosthesis removal may also be required.
Last updated: Dec 15, 2025
The majority of septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease are monomicrobial. Common organisms include:
| Risk factors | Infectious agents |
|---|---|
| No specific risk factor | S. aureus S. aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Staphylococcus |
| Prosthetic joint replacement Prosthetic Joint Replacement Septic Arthritis |
|
| Chronic disease, autoimmune disorder Autoimmune Disorder Septic Arthritis, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions infection, trauma, elderly | S. pyogenes (group A beta-hemolytic strep) |
| Young, sexually active | N. gonorrhoeae N. gonorrhoeae A species of gram-negative, aerobic bacteria primarily found in purulent venereal discharges. It is the causative agent of gonorrhea. Neisseria |
| Trauma |
|
| Sickle cell anemia Sickle cell anemia A disease characterized by chronic hemolytic anemia, episodic painful crises, and pathologic involvement of many organs. It is the clinical expression of homozygosity for hemoglobin S. Sickle Cell Disease |
|
| Immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis, IV drug use |
|
Joints can be inoculated in different ways. Infecting organisms multiply in the synovial fluid and synovial lining.[1,5]
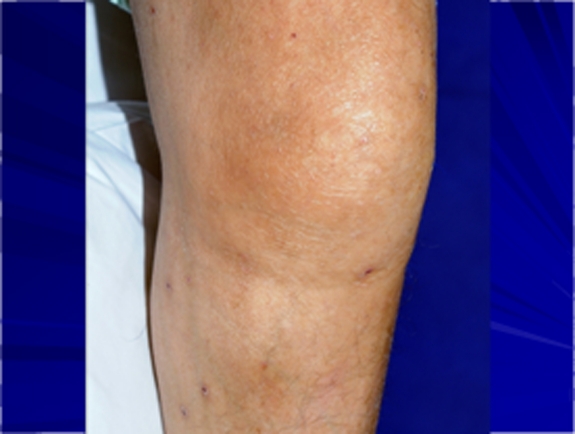
Knee swelling and mild erythema in a patient with septic arthritis
Image: “Troublesome Tuberculosis: A Case Report on Multi-focal Tuberculous Osteomyelitis in An Immunocompetent Patient” by Lynn MM, Kukanesen JR, Khan AW. License: CC BY 2.0
Significant erythema and swelling over the right sternoclavicular joint, which is concerning for septic arthritis
Image: “Sternoclavicular joint septic arthritis with chest wall abscess in a healthy adult: a case report” by Tanaka Y, Kato H, Shirai K, Nakajima Y, Yamada N, Okada H, Yoshida T, Toyoda I, Ogura S. License: CC BY 4.0The diagnosis of septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis is made with synovial fluid analysis Synovial Fluid Analysis Rheumatoid Arthritis.
| Normal | Noninflammatory (e.g., osteoarthritis Osteoarthritis Osteoarthritis (OA) is the most common form of arthritis, and is due to cartilage destruction and changes of the subchondral bone. The risk of developing this disorder increases with age, obesity, and repetitive joint use or trauma. Patients develop gradual joint pain, stiffness lasting < 30 minutes, and decreased range of motion. Osteoarthritis) | Inflammatory (e.g., rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis) | Septic | |
|---|---|---|---|---|
| Clarity | Clear | Translucent | Opaque | |
| Color | Clear/straw | Straw/yellow | Yellow/milky | Milky/yellow/green |
| WBC (cells/μL) | < 2,000 | 2,000–20,000 | > 20,000* | |
| Percent neutrophils Neutrophils Granular leukocytes having a nucleus with three to five lobes connected by slender threads of chromatin, and cytoplasm containing fine inconspicuous granules and stainable by neutral dyes. Innate Immunity: Phagocytes and Antigen Presentation | < 25 | 50%–75% | > 75% | |
| Stain/culture | Negative | Usually positive | ||
Laboratory studies that support the diagnosis:

X-ray showing soft-tissue swelling of the right ankle in an 8-month-old patient with septic arthritis
Image: “Polyarticular Septic Arthritis Caused by Haemophilus influenzae Serotype f in an 8-Month-Old Immunocompetent Infant: A Case Report and Review of the Literature” by Ali RA, Kaplan SL, Rosenfeld SB. License: CC BY 3.0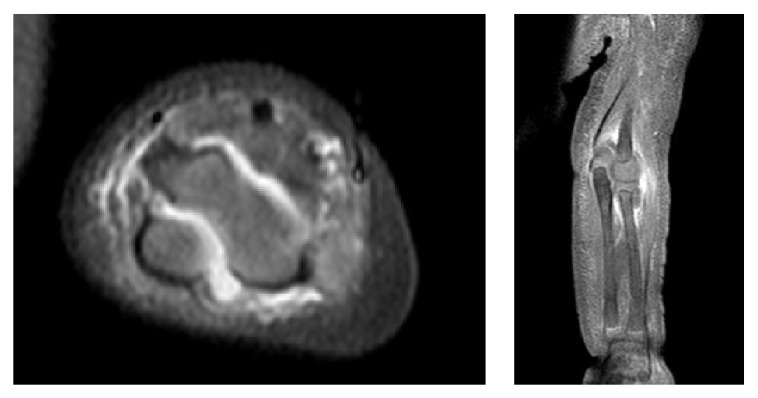
MRI showing a large effusion between the humerus and olecranon process in a pediatric patient with septic arthritis
Image: “Polyarticular Septic Arthritis Caused by Haemophilus influenzae Serotype f in an 8-Month-Old Immunocompetent Infant: A Case Report and Review of the Literature” by Ali RA, Kaplan SL, Rosenfeld SB. License: CC BY 3.0
X-ray of the knee demonstrating mild periarticular osteopenia and significant joint-space narrowing in a patient with septic arthritis
Image: “Disseminated Aspergillus flavus following septic arthritis in an immunocompetent patient: a case report” by Tiwari V, Khatri K, Khan SA, Nath D. License: CC BY 4.0
Ultrasound of the right shoulder glenohumeral articulation showing a distended posterior aspect of joint capsule by fluid (A) in a patient with septic arthritis
Image: “Streptococcus agalactiae Septic Arthritis of the Shoulder and the Sacroiliac Joints: A Case Report” by Imam YZ, Sarakbi HA, Abdelwahab N, Mattar I. License: CC BY 3.0Components of management include: (1) early identification Identification Defense Mechanisms and treatment, (2) antibiotic therapy, and (3) joint aspiration/drainage (with orthopedic consultation, as indicated).
Antibiotic selection Selection Lymphocyte activation by a specific antigen thus triggering clonal expansion of lymphocytes already capable of mounting an immune response to the antigen. B cells: Types and Functions is based on the initial Gram stain Gram stain Klebsiella and tailored based on culture data. Rapid joint destruction can occur in septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis (of a native joint), so broad-spectrum Broad-Spectrum Fluoroquinolones antibiotic coverage is often required initially.
Empiric regimen if Gram stain Gram stain Klebsiella is negative (no organism seen, but synovial fluid cell count elevated):[6,9,11,13,16–21]
Gram-positive Gram-Positive Penicillins cocci Cocci Bacteriology:[6,10,11,13,22–29]
Gram-negative bacilli Bacilli Shigella:[11,13,30]
Gram-negative cocci Cocci Bacteriology:[6,9,11,13]
| Causative pathogen | Suggested empiric regimen | |
|---|---|---|
| Gram-negative (no organisms) | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections (assess need with Pseudomonas Pseudomonas Pseudomonas is a non-lactose-fermenting, gram-negative bacillus that produces pyocyanin, which gives it a characteristic blue-green color. Pseudomonas is found ubiquitously in the environment, as well as in moist reservoirs, such as hospital sinks and respiratory equipment. Pseudomonas coverage based on risks) | |
| Gram-positive Gram-Positive Penicillins cocci Cocci Bacteriology |
|
|
| Gram-negative cocci Cocci Bacteriology |
|
|
| Gram-negative bacilli Bacilli Shigella | Immunocompetent (no risk for Pseudomonas Pseudomonas Pseudomonas is a non-lactose-fermenting, gram-negative bacillus that produces pyocyanin, which gives it a characteristic blue-green color. Pseudomonas is found ubiquitously in the environment, as well as in moist reservoirs, such as hospital sinks and respiratory equipment. Pseudomonas) | 3rd-generation cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections (e.g., ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins, cefotaxime Cefotaxime Semisynthetic broad-spectrum cephalosporin. Cephalosporins) |
| Immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis (with risk for Pseudomonas Pseudomonas Pseudomonas is a non-lactose-fermenting, gram-negative bacillus that produces pyocyanin, which gives it a characteristic blue-green color. Pseudomonas is found ubiquitously in the environment, as well as in moist reservoirs, such as hospital sinks and respiratory equipment. Pseudomonas) | Ceftazidime Ceftazidime Semisynthetic, broad-spectrum antibacterial derived from cephaloridine and used especially for pseudomonas and other gram-negative infections in debilitated patients. Cephalosporins, cefepime Cefepime A fourth-generation cephalosporin antibacterial agent that is used in the treatment of infections, including those of the abdomen, urinary tract, respiratory tract, and skin. It is effective against pseudomonas aeruginosa and may also be used in the empiric treatment of febrile neutropenia. Cephalosporins | |
Duration of therapy depends on additional factors:[6]
Antibiotics for PJI:[7,14]
Joint drainage Joint Drainage Septic Arthritis:[5–7]
Surgical debridement Debridement The removal of foreign material and devitalized or contaminated tissue from or adjacent to a traumatic or infected lesion until surrounding healthy tissue is exposed. Stevens-Johnson Syndrome in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with prosthesis:[6,14]
This list of complications is not exhaustive.
Diagnosis Codes:
These codes are used to diagnose septic
arthritis
Arthritis
Acute or chronic inflammation of joints.
Osteoarthritis, a serious infection in a joint. The codes are specific to the causative organism (e.g., Staphylococcal) and the affected joint (e.g., the knee).
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | M00.061 | Staphylococcal arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, right knee |
| ICD-10-CM | M00.9 | Pyogenic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis, unspecified |
Evaluation & Workup:
This CPT code is for an
arthrocentesis
Arthrocentesis
Puncture and aspiration of fluid (e.g., synovial fluid) from a joint cavity. It is used sometimes to irrigate or administer drugs into a joint cavity.
Septic Arthritis, the essential diagnostic procedure for septic
arthritis
Arthritis
Acute or chronic inflammation of joints.
Osteoarthritis, which involves aspirating synovial fluid from the joint for cell count,
Gram stain
Gram stain
Klebsiella, and culture.
| Coding System | Code | Description |
|---|---|---|
| CPT | 20610 | Arthrocentesis Arthrocentesis Puncture and aspiration of fluid (e.g., synovial fluid) from a joint cavity. It is used sometimes to irrigate or administer drugs into a joint cavity. Septic Arthritis, aspiration and/or injection, major joint or bursa; without ultrasound guidance |
Medications:
This code is for a
broad-spectrum
Broad-Spectrum
Fluoroquinolones antibiotic like
vancomycin
Vancomycin
Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear.
Glycopeptides, which is often started empirically as intravenous therapy to cover for
Methicillin-resistant Staphylococcus aureus
Methicillin-Resistant Staphylococcus Aureus
Multidrug-resistant Organisms and Nosocomial Infections (
MRSA
MRSA
A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins.
Staphylococcus) pending culture results.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 11124 | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides (ingredient) |