The scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy is a sac hanging outside the body that contains parts of the male reproductive system. The scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy’s main function is to support testicles Testicles The testicles, also known as the testes or the male gonads, are a pair of egg-shaped glands suspended within the scrotum. The testicles have multiple layers: an outer tunica vaginalis, an intermediate tunica albuginea, and an innermost tunica vasculosa. The testicles are composed of testicular lobules and seminiferous tubules. Testicles: Anatomy outside the body so that spermatogenesis Spermatogenesis The process of germ cell development in the male from the primordial germ cells, through spermatogonia; spermatocytes; spermatids; to the mature haploid spermatozoa. Gametogenesis can be completed under optimal conditions. The scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy can be affected by various pathologic conditions, and imaging is a valuable tool in reaching the appropriate diagnosis. The most important imaging method is ultrasonography +/– Doppler Doppler Ultrasonography applying the doppler effect, with frequency-shifted ultrasound reflections produced by moving targets (usually red blood cells) in the bloodstream along the ultrasound axis in direct proportion to the velocity of movement of the targets, to determine both direction and velocity of blood flow. Ultrasound (Sonography) mode because scrotal structures are superficial with no intervening gas. MRI is useful when ultrasound is indeterminate.
Last updated: Dec 15, 2025
Ultrasonography is often the best imaging method for the scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy.
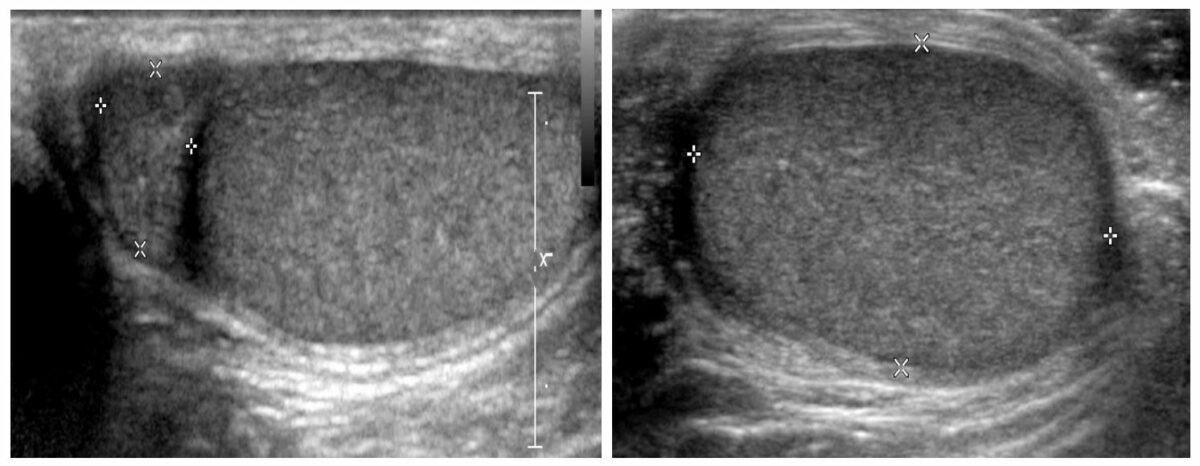
Scrotal ultrasonogram showing the testicle (with a homogeneous echotexture with no focal lesions or surrounding fluid) and the epididymis
Image by Hetal Verma, MD.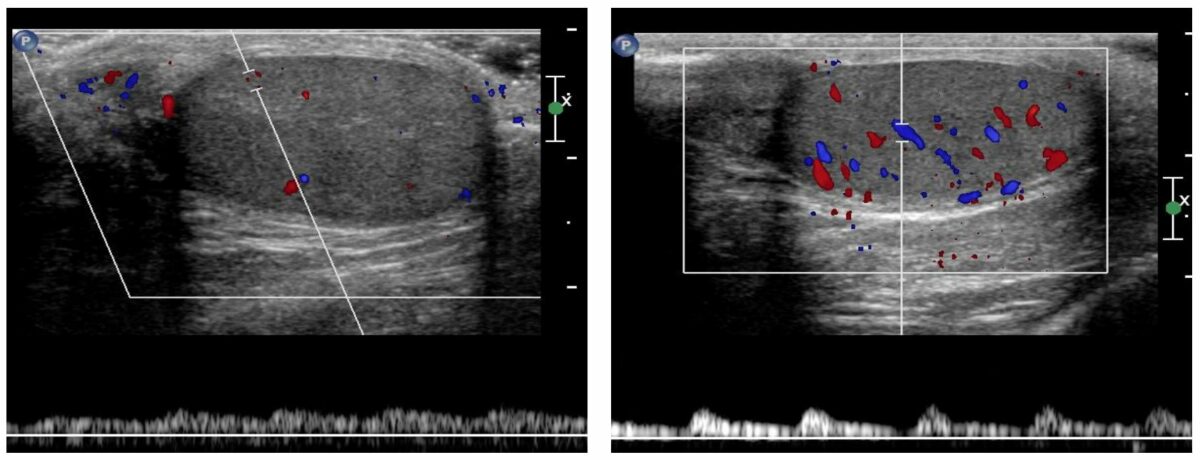
Doppler ultrasound showing normal arterial and venous flow with normal venous (left image) and arterial (right image) waveforms
Image by Hetal Verma, MD.Ultrasound findings include:
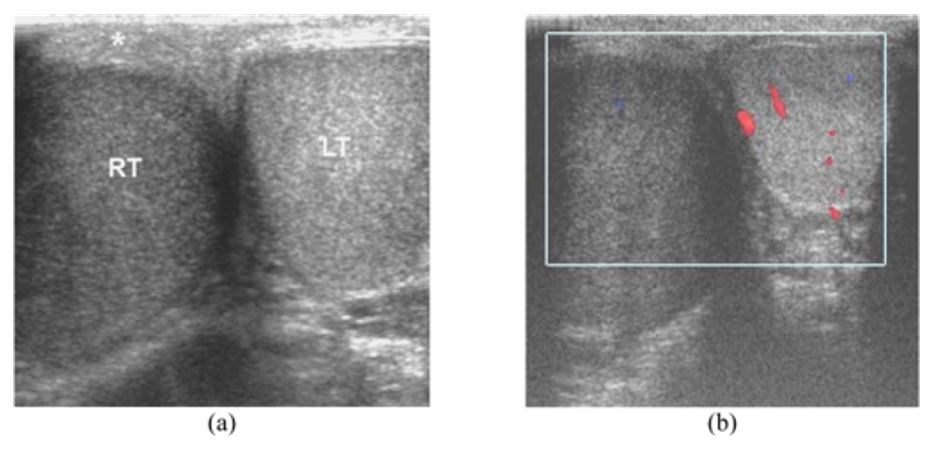
Epididymo-orchitis in a 45-year-old man presenting with painful swelling of the right hemiscrotum for 3 days:
a: Transverse ultrasonogram of the scrotum shows an enlarged hypoechoic right testis (RT) and a normal left testis (LT). The overlying right scrotal skin is thickened (asterisk).
b: Longitudinal color Doppler ultrasonogram of the right hemiscrotum shows increased vascular flow in the right epididymis and testis.
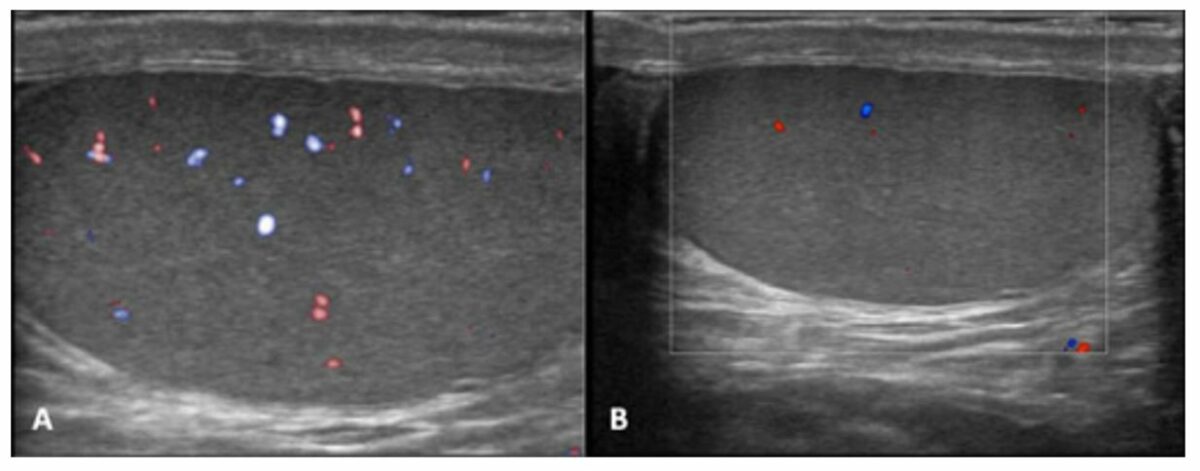
Orchitis:
Color Doppler shows increased flow in the left testis (arrow) with normal color flow in the right testis.

Tuberculous epididymo-orchitis in a 39-year-old man with a history of pulmonary tuberculosis, presenting with chronic painless left testicular swelling for 3 years:
Composite ultrasonogram of the left hemiscrotum show a nodular, enlarged heterogeneously hypoechoic epididymal head (HE) and tail (TE), and heterogeneously echoic testis (T).
Ultrasound findings include:
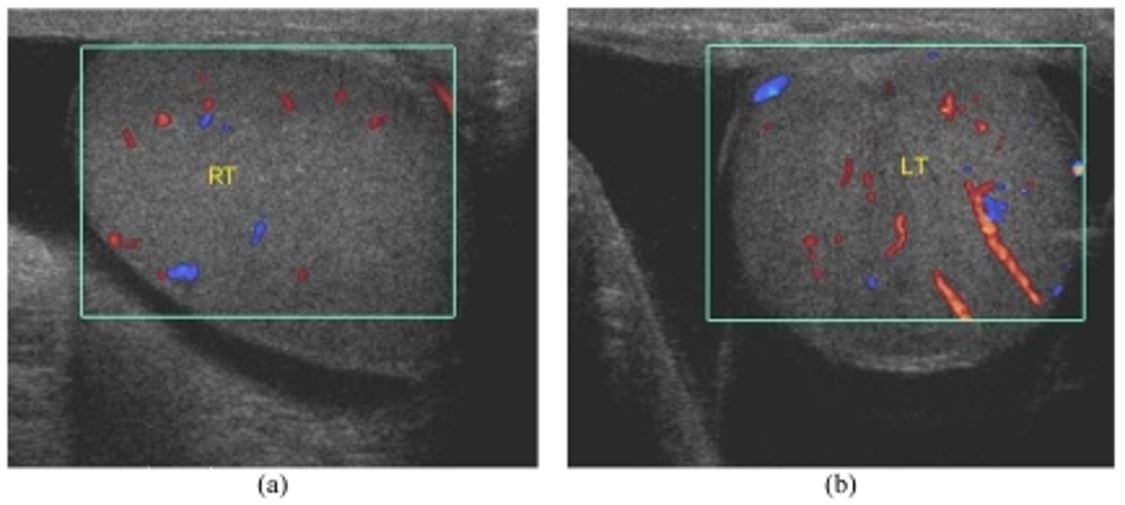
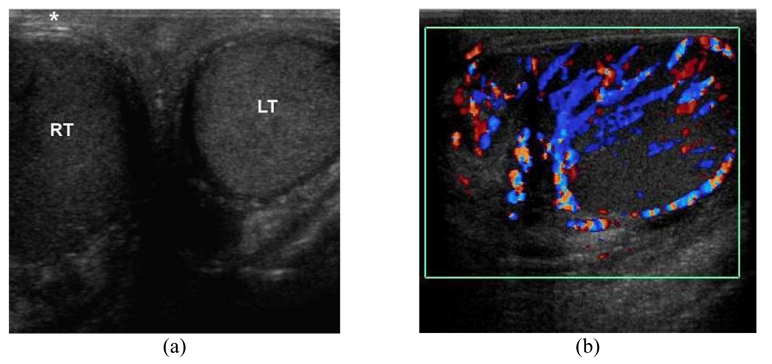
Bilateral hydrocele in a 58-year-old man with a history of progressive painless swelling of bilateral hemiscrotum for 2 years:
Oblique color Doppler images show anechoic fluid surrounding the testes, left more than right. There is normal vascular flow in both the right (RT) and left (LT) testes.
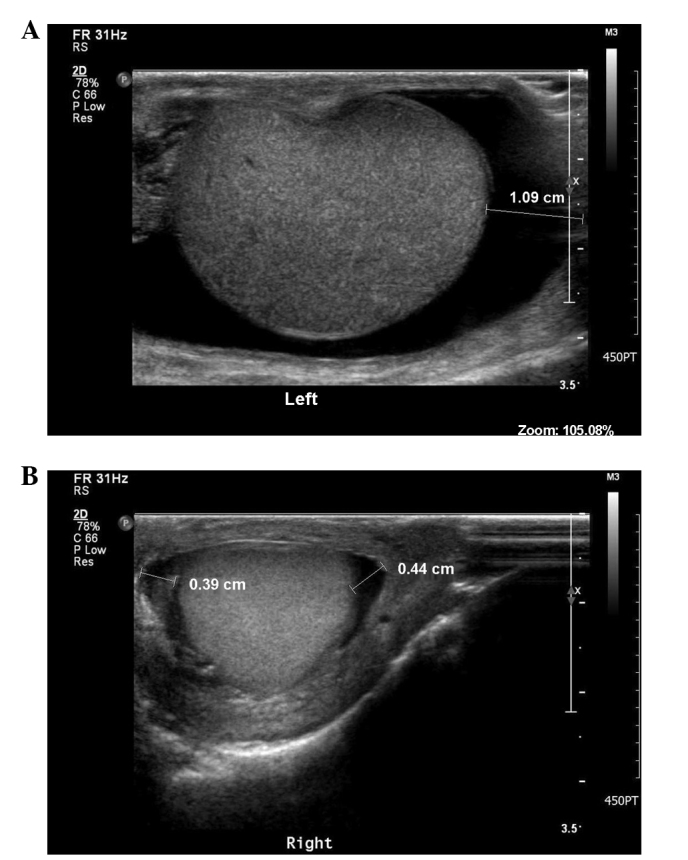
Metastatic testicular tumor presenting as a scrotal hydrocele:
Scrotal ultrasonography findings showing (A) a large amount of fluid in the left scrotal sac and (B) a small amount of fluid with internal echogenic material in the right scrotal sac, indicating bilateral hydroceles
Ultrasound findings include:
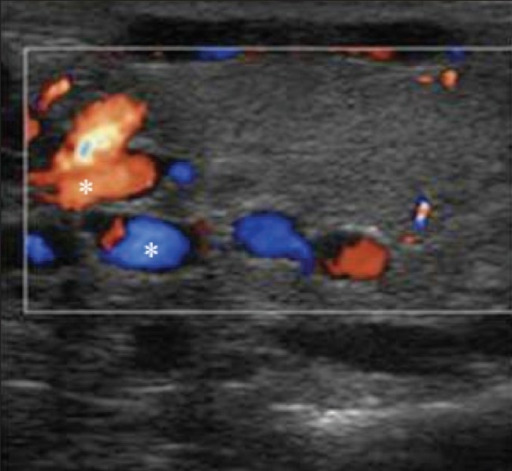
Varicoceles color Doppler shows a venous pattern of color flow in the anechoic channels (asterisk) confirming the diagnosis of both intratesticular and extratesticular varicoceles.
Image: “Varicoceles Color Doppler” by Patiala B. License: CC BY 2.0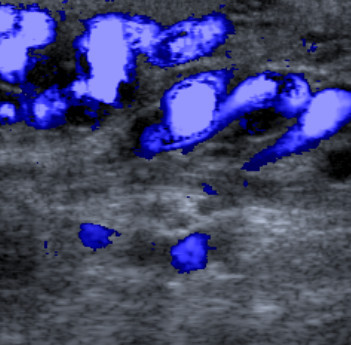
Color Doppler ultrasound image:
Variceal gonadal vein in the left inguinal canal
Ultrasound findings:
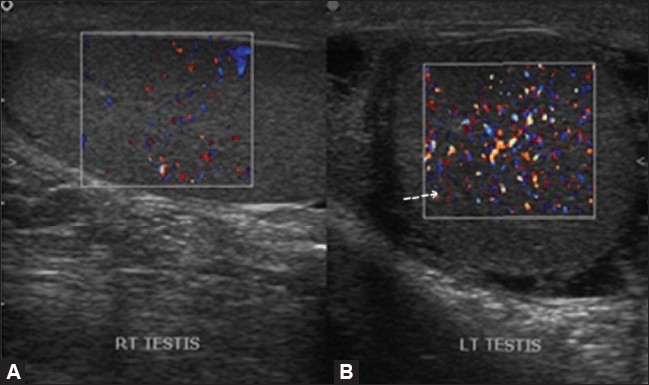
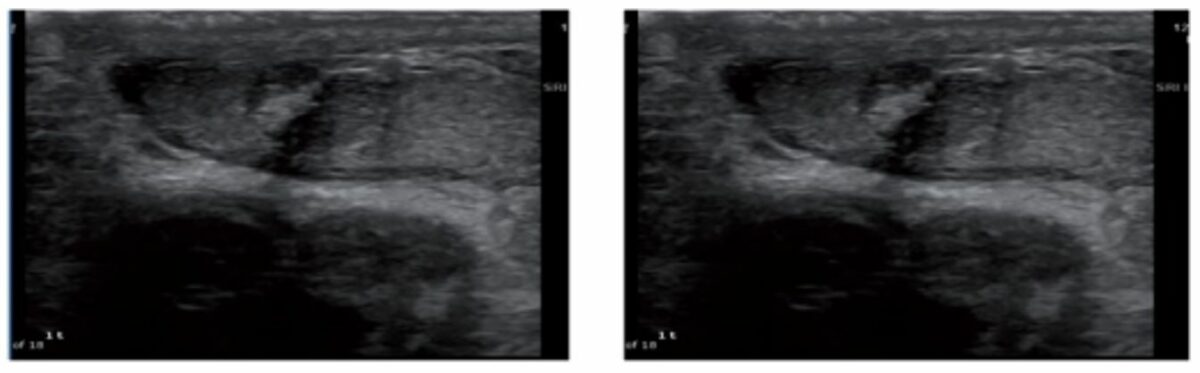
Gray-scale and color Doppler of testicular torsion:
In the early phases of torsion (1–3 hours), testicular echogenicity appears normal. With progression, enlargement of the affected testis and increased or heterogeneous echogenicity are common findings.
Ultrasound findings include:
Leydig cell tumor:
Heterogeneous mass in which malignancy was suspected, eventually found to be Leydig cell tumor with similar size estimated preoperatively
| Structure | T1-weighted | T2-weighted | With contrast |
|---|---|---|---|
| Testicle ( homogeneous Homogeneous Imaging of the Spleen oval structure) | Hypointense Hypointense Magnetic Resonance Imaging (MRI) to isointense | Hyperintense Hyperintense Magnetic Resonance Imaging (MRI) | Enhance |
| Epididymis Epididymis The convoluted cordlike structure attached to the posterior of the testis. Epididymis consists of the head (caput), the body (corpus), and the tail (cauda). A network of ducts leaving the testis joins into a common epididymal tubule proper which provides the transport, storage, and maturation of spermatozoa. Testicles: Anatomy | Isointense | Hypointense Hypointense Magnetic Resonance Imaging (MRI) | Enhance |
| Tunica albuginea Tunica albuginea Penis: Anatomy | Hypointense Hypointense Magnetic Resonance Imaging (MRI) | Hypointense Hypointense Magnetic Resonance Imaging (MRI) | Not applicable |
MRI findings include:

Transverse T1-weighted image depicts a multilobular left scrotal mass (short arrow), located in the paratesticular space.
The lesion had similar signal intensity when compared with the normal testicular parenchyma (asterisk).
Left hydrocele (long arrow)