Rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis (RA) is a symmetric, inflammatory polyarthritis and chronic, progressive, autoimmune disorder Autoimmune Disorder Septic Arthritis. Presentation occurs most commonly in middle-aged women with joint swelling Swelling Inflammation, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, and morning stiffness (often in the hands). Systemic inflammation Systemic Inflammation Surgical Site Infections can lead to extraarticular manifestations such as rheumatoid nodules, interstitial lung disease, Felty syndrome, and pericarditis Pericarditis Pericarditis is an inflammation of the pericardium, often with fluid accumulation. It can be caused by infection (often viral), myocardial infarction, drugs, malignancies, metabolic disorders, autoimmune disorders, or trauma. Acute, subacute, and chronic forms exist. Pericarditis. Prolonged and severe disease can lead to irreversible joint deformities. Diagnosis is based on strong clinical suspicion and confirmed by the presence of rheumatoid factor Rheumatoid factor Antibodies found in adult rheumatoid arthritis patients that are directed against gamma-chain immunoglobulins. Autoimmune Hepatitis (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies Antibodies Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various Ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, and characteristic imaging. Management involves long-term disease-modifying antirheumatic drugs Disease-modifying antirheumatic drugs Disease-modifying antirheumatic drugs are antiinflammatory medications used to manage rheumatoid arthritis. The medications slow, but do not cure, the progression of the disease. The medications are classified as either synthetic or biologic agents and each has unique mechanisms of action and side effects. Disease-Modifying Antirheumatic Drugs (DMARDs) ( DMARDs DMARDs Disease-modifying antirheumatic drugs are antiinflammatory medications used to manage rheumatoid arthritis. The medications slow, but do not cure, the progression of the disease. The medications are classified as either synthetic or biologic agents and each has unique mechanisms of action and side effects. Disease-Modifying Antirheumatic Drugs (DMARDs)), biologic agents Biologic Agents Immunosuppressants, and physical therapy Physical Therapy Becker Muscular Dystrophy. Glucocorticoids Glucocorticoids Glucocorticoids are a class within the corticosteroid family. Glucocorticoids are chemically and functionally similar to endogenous cortisol. There are a wide array of indications, which primarily benefit from the antiinflammatory and immunosuppressive effects of this class of drugs. Glucocorticoids and nonsteroidal antiinflammatory drugs Nonsteroidal Antiinflammatory Drugs Nonsteroidal antiinflammatory drugs (NSAIDs) are a class of medications consisting of aspirin, reversible NSAIDs, and selective NSAIDs. NSAIDs are used as antiplatelet, analgesic, antipyretic, and antiinflammatory agents. Nonsteroidal Antiinflammatory Drugs (NSAIDs) ( NSAIDs NSAIDS Primary vs Secondary Headaches) are the treatment of choice for acute exacerbation.
Last updated: Dec 15, 2025
The cause of rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis (RA) is unknown, but several risk factors play a role.
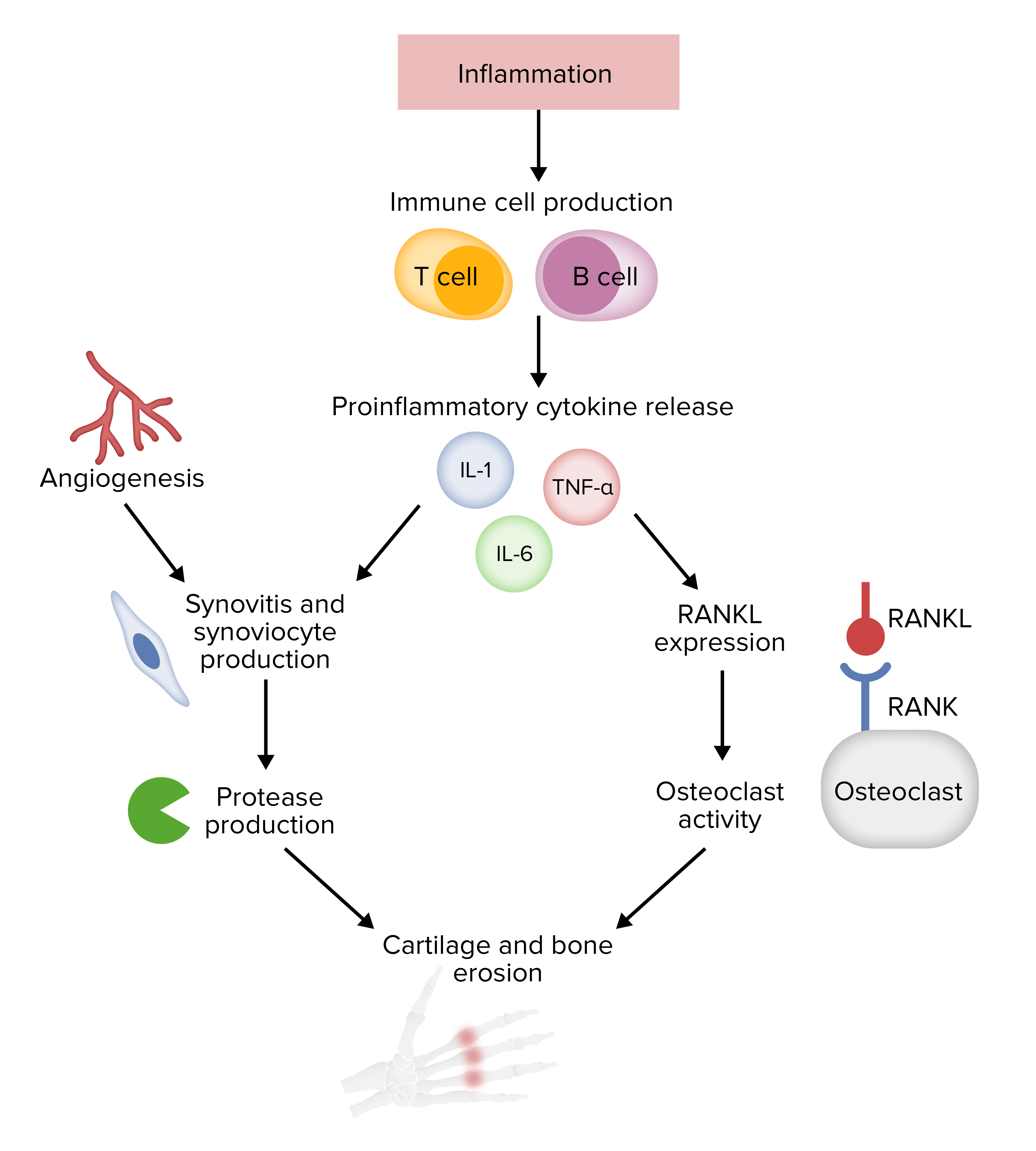
Pathophysiology of rheumatoid arthritis
RANK: receptor activator of nuclear factor kappa-Β
RANKL: receptor activator of nuclear factor kappa-Β ligand
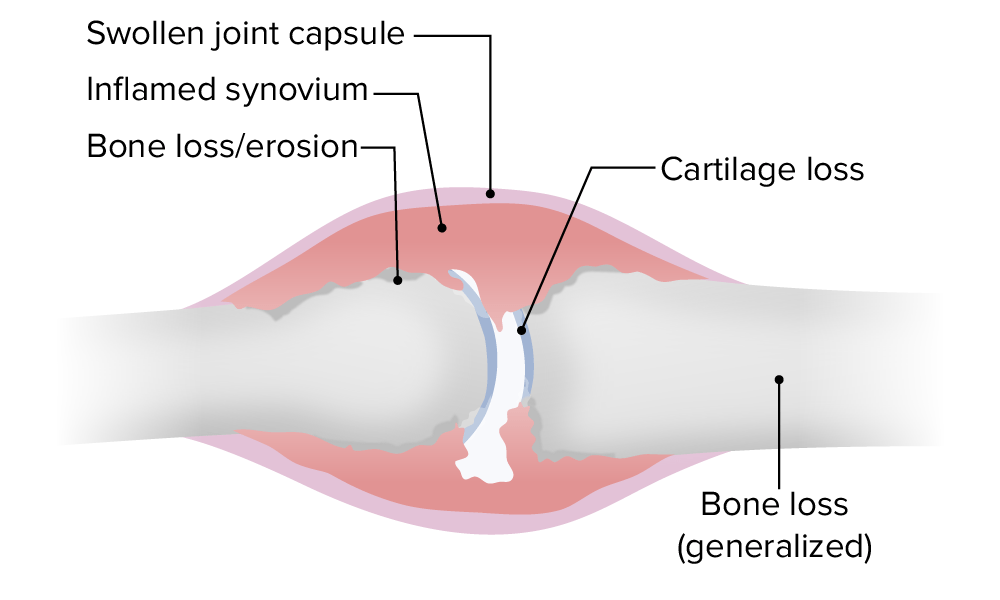
The pathological joint changes in rheumatoid arthritis
Image by Lecturio.
Arthroscopic images in RA: Exuberant synovial growth with villi-like proliferation
Image: “Arthroscopic image of synovial growth” by Department of Orthopaedics, Grant Government Medical College & Sir J.J. Group of Hospitals, Byculla, Mumbai, India. License: CC BY 4.0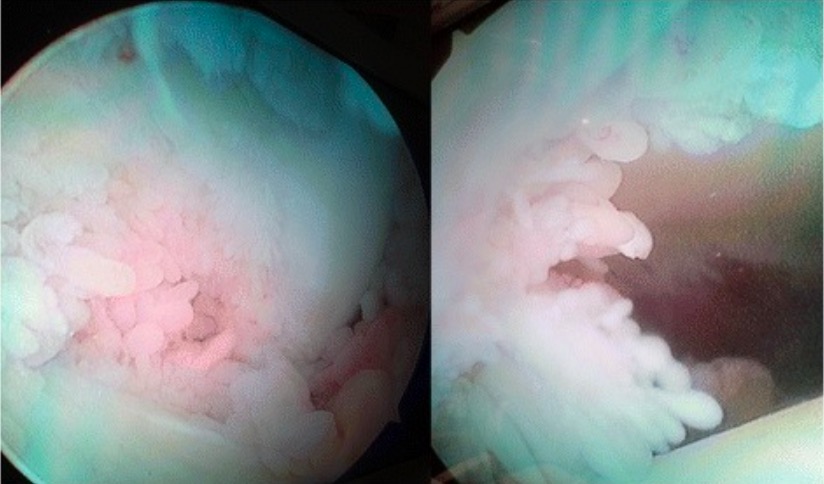
Arthroscopic image of synovial proliferation of the knee in a patient with RA
Image: “Arthroscopic image of synovial growth” by Department of Orthopaedics, Grant Government Medical College & Sir J.J. Group of Hospitals, Byculla, Mumbai, India. License: CC BY 4.0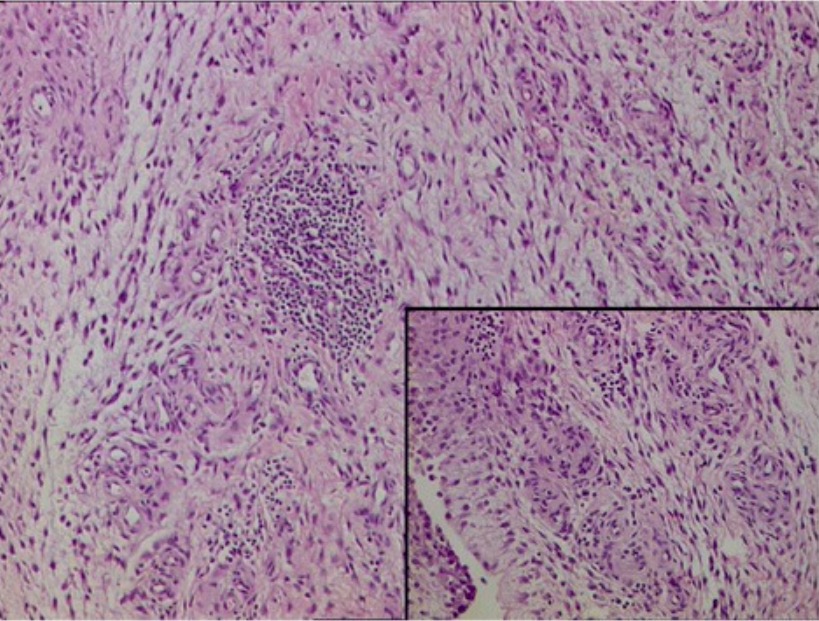
Histopathology of the synovium in RA: Fibrocollagenous tissue with dense, mixed inflammatory infiltrate comprised of lymphocytes, plasma cells, neutrophils, and proliferative blood vessels
Image: “Histopathology” by Department of Orthopaedics, Grant Government Medical College & Sir J.J. Group of Hospitals, Byculla, Mumbai, India. License: CC BY 4.0
Swan neck deformity of the fifth finger in a patient with RA
Image: “Swan-neck deformity” by Khatam-al-Anbia Eye Research Center, Mashhad University of Medical Sciences, Mashhad, Iran. License: CC BY 2.5
Synovitis in RA:
Presentation includes symmetric swelling and tenderness of MCP joints, PIP joints, and wrists.

Physical exam findings in RA:
An RA patient with several classic deformities: ulnar deviation (left hand) and Boutonniere deformity (3rd, 4th, and 5th fingers of the right hand)

Rheumatoid nodules in RA:
Firm, non-tender, subcutaneous swelling on the extensor surface of the elbow in a RA patient
Rheumatoid arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis (RA) diagnosis is based on high clinical suspicion and confirmed by serology Serology The study of serum, especially of antigen-antibody reactions in vitro. Yellow Fever Virus and imaging.

Radiograph of the hands in a patient with RA:
“Z” deformity shown in both thumbs and joint-space narrowing/bony erosion noted in CMC, MCP, and PIP joints
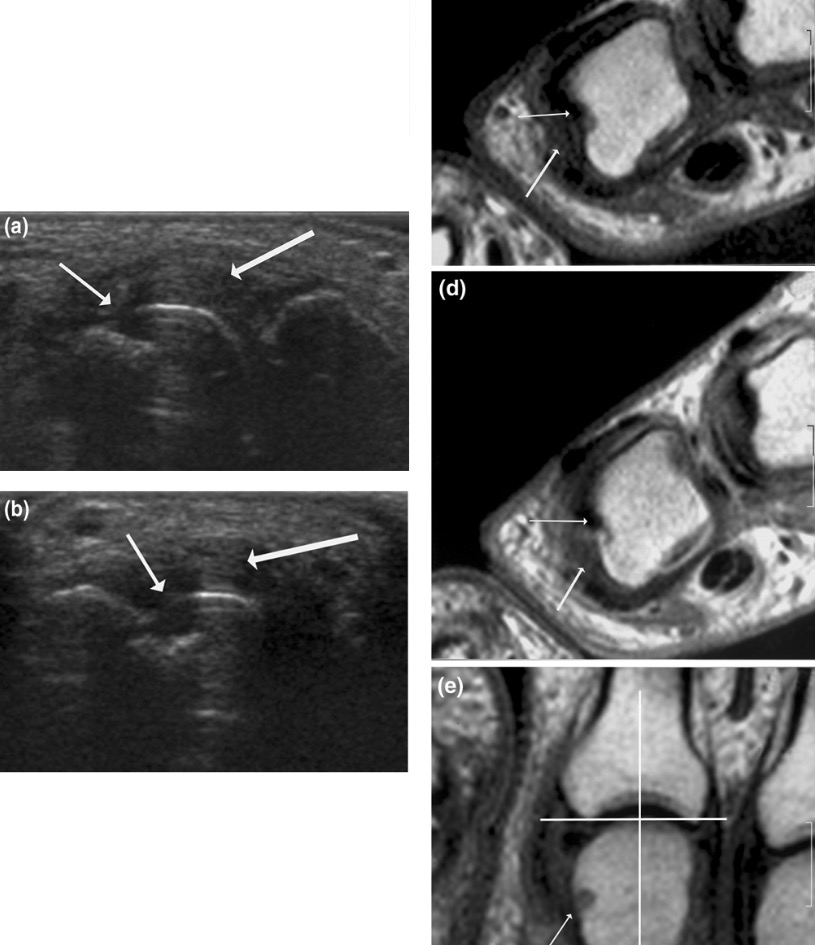
Ultrasound and MRI findings in RA:
(a) (b): Signs of destruction and inflammation on ultrasonography
(c) (d) (e): Magnetic resonance imaging showing 2nd MCP joint in a patient with established RA.
(thin arrows indicate erosive change; thick arrows indicate synovitis)
The goal is to prevent deformity Deformity Examination of the Upper Limbs and permanent damage. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship should be referred to a rheumatologist.
Nonpharmacological therapies:
Acute exacerbation management:
Long-term pharmacological therapy:
Surgery:
Additional considerations: