Reactive arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis is a seronegative immune-mediated spondyloarthritis that occurs in response to a previous gastrointestinal (GI) or genitourinary (GU) infection. The pathophysiology of this disease is unclear, but a significant proportion of affected patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are positive for HLA-B27. The disease manifests as asymmetric oligoarthritis Oligoarthritis Ankylosing Spondylitis (particularly of large joints in the lower extremities), enthesopathy, dactylitis Dactylitis Ankylosing Spondylitis, and/or sacroiliitis Sacroiliitis Inflammation of the sacroiliac joint. It is characterized by lower back pain, especially upon walking, fever, uveitis; psoriasis; and decreased range of motion. Many factors are associated with and cause sacroiliitis including infection; injury to spine, lower back, and pelvis; degenerative arthritis; and pregnancy. Ankylosing Spondylitis. Ocular, mucocutaneous, GI, GU, and cardiac manifestations may also occur. The diagnosis is clinical, and efforts should be made to rule out alternative diagnoses. Management focuses on controlling symptoms, typically with nonsteroidal anti-inflammatory drugs. An active infection should also be treated, particularly Chlamydia trachomatis Chlamydia trachomatis Type species of Chlamydia causing a variety of ocular and urogenital diseases. Chlamydia.
Last updated: Dec 15, 2025
Reactive arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis (ReA) is an immune-mediated, post-infectious, seronegative spondyloarthritis.
The seronegative arthropathies Seronegative Arthropathies Ankylosing Spondylitis can be remembered as “PAIR.”
Onset is acute, within 1–4 weeks of an inciting infection.
Peripheral arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis:
Enthesopathy:
Tendonitis and periostitis:
Dactylitis Dactylitis Ankylosing Spondylitis:
Sacroiliitis Sacroiliitis Inflammation of the sacroiliac joint. It is characterized by lower back pain, especially upon walking, fever, uveitis; psoriasis; and decreased range of motion. Many factors are associated with and cause sacroiliitis including infection; injury to spine, lower back, and pelvis; degenerative arthritis; and pregnancy. Ankylosing Spondylitis:
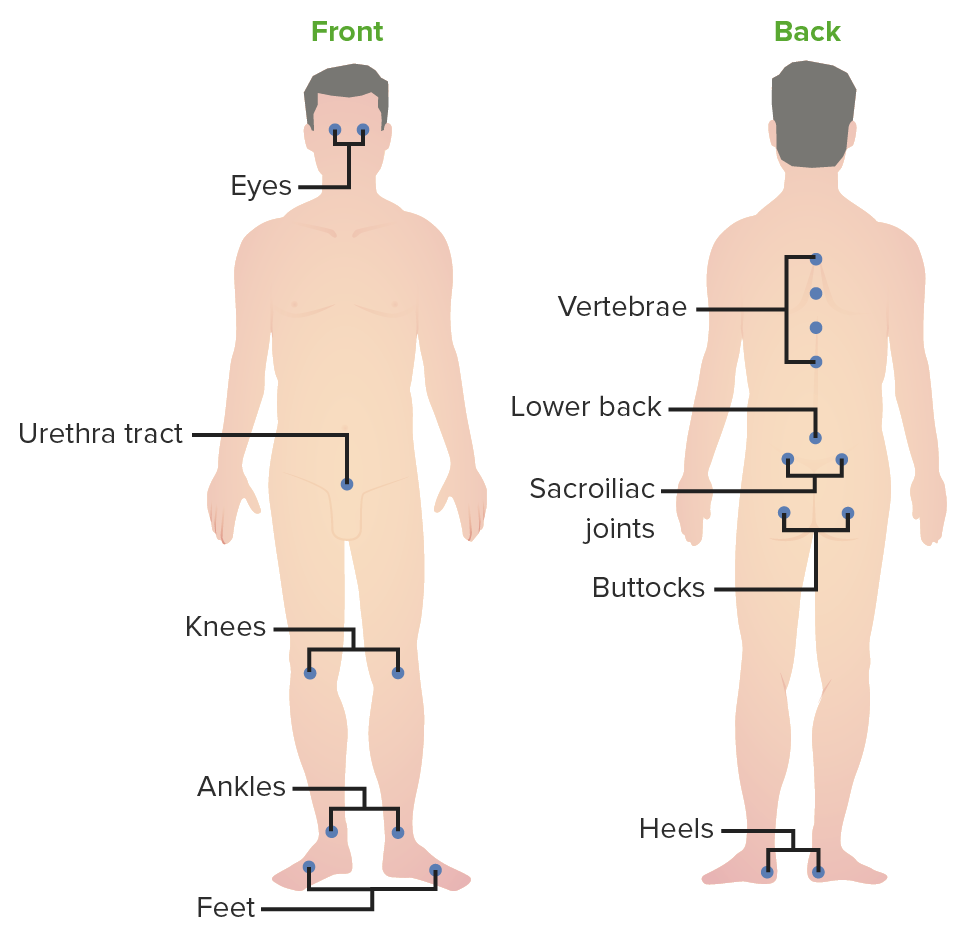
Common inflammatory sites in ReA: Image demonstrates the common joints involved in ReA. Conjunctivitis and urethritis are also frequent manifestations, and are part of the clinical triad for ReA.
Image by Lecturio.Ocular:
Genitourinary:
Mucocutaneous:
GI:
Cardiac:

Presentation of acute viral conjunctivitis:
Conjunctivitis, which is typically seen with viral infection of the pharynx

Keratoderma blennorrhagicum:
A cutaneous manifestation of reactive arthritis, which commonly affects the palms and soles

Balanitis circinata:
Another possible extra-articular manifestation of reactive arthritis.
This classic triad of symptoms is found in only about 30% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with ReA:
Reactive arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis is a clinical diagnosis based on:
Synovial fluid analysis Synovial Fluid Analysis Rheumatoid Arthritis:
Laboratory findings:
Radiographs of affected joints:
Symptoms of ReA typically resolve in 3‒4 months, but prolonged or recurrent symptoms can occur in up to 50% of patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship.
Acute ReA (duration < 6 months):
Chronic ReA (duration > 6 months):
Ocular:
Mucocutaneous: