Rapidly progressive glomerulonephritis (RPGN) is a syndrome of severe glomerular disease with progressive loss of kidney function within weeks to months. Rapidly progressive glomerulonephritis is associated with nephritic syndrome Nephritic syndrome Nephritic syndrome is a broad category of glomerular diseases characterized by glomerular hematuria, variable loss of renal function, and hypertension. These features are in contrast to those of nephrotic syndrome, which includes glomerular diseases characterized by severe proteinuria, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephritic Syndrome and is a manifestation of different diseases. Histologically, crescents (the proliferation of epithelial cells and the infiltration of monocytes Monocytes Large, phagocytic mononuclear leukocytes produced in the vertebrate bone marrow and released into the blood; contain a large, oval or somewhat indented nucleus surrounded by voluminous cytoplasm and numerous organelles. Innate Immunity: Phagocytes and Antigen Presentation/ macrophages Macrophages The relatively long-lived phagocytic cell of mammalian tissues that are derived from blood monocytes. Main types are peritoneal macrophages; alveolar macrophages; histiocytes; kupffer cells of the liver; and osteoclasts. They may further differentiate within chronic inflammatory lesions to epithelioid cells or may fuse to form foreign body giant cells or langhans giant cells. Innate Immunity: Phagocytes and Antigen Presentation in the Bowman space) are found in the glomeruli and arise from immunologic injury. The major mechanisms of immunologic injury are classified into anti-glomerular basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN) (anti-GBM) disease, pauci-immune crescentic glomerulonephritis, and immune complex-mediated injury. Rapidly progressive glomerulonephritis can manifest with hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma, proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children, and varying degrees of edema Edema Edema is a condition in which excess serous fluid accumulates in the body cavity or interstitial space of connective tissues. Edema is a symptom observed in several medical conditions. It can be categorized into 2 types, namely, peripheral (in the extremities) and internal (in an organ or body cavity). Edema and hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. Diagnosis is by presentation, laboratory tests, imaging, and renal biopsy Renal Biopsy Antineutrophil Cytoplasmic Antibody (ANCA)-Associated Vasculitis. Prompt treatment is essential because RPGN can develop into end-stage renal disease within a short period of time. Modalities include corticosteroids Corticosteroids Chorioretinitis, cyclophosphamide Cyclophosphamide Precursor of an alkylating nitrogen mustard antineoplastic and immunosuppressive agent that must be activated in the liver to form the active aldophosphamide. It has been used in the treatment of lymphoma and leukemia. Its side effect, alopecia, has been used for defleecing sheep. Cyclophosphamide may also cause sterility, birth defects, mutations, and cancer. Immunosuppressants or other immunosuppressants Immunosuppressants Immunosuppressants are a class of drugs widely used in the management of autoimmune conditions and organ transplant rejection. The general effect is dampening of the immune response. Immunosuppressants, and plasmapheresis Plasmapheresis Procedure whereby plasma is separated and extracted from anticoagulated whole blood and the red cells retransfused to the donor. Plasmapheresis is also employed for therapeutic use. Stevens-Johnson Syndrome (depending on the underlying disease).
Last updated: May 17, 2024
Rapidly progressive glomerulonephritis (RPGN) is a syndrome of severe glomerular disease with progressive loss of kidney function within weeks to months.
Most cases are from immunological injury of the glomeruli. The mechanisms and findings are classified as:
| Condition | Light microscopy | Fluorescence microscopy | Electron microscopy |
|---|---|---|---|
| Anti-glomerular basement membrane Basement membrane A darkly stained mat-like extracellular matrix (ecm) that separates cell layers, such as epithelium from endothelium or a layer of connective tissue. The ecm layer that supports an overlying epithelium or endothelium is called basal lamina. Basement membrane (bm) can be formed by the fusion of either two adjacent basal laminae or a basal lamina with an adjacent reticular lamina of connective tissue. Bm, composed mainly of type IV collagen; glycoprotein laminin; and proteoglycan, provides barriers as well as channels between interacting cell layers. Thin Basement Membrane Nephropathy (TBMN) (anti-GBM) disease |
|
Linear IgG IgG The major immunoglobulin isotype class in normal human serum. There are several isotype subclasses of igg, for example, igg1, igg2a, and igg2b. Hypersensitivity Pneumonitis and C3 |
|
| Immune complex-mediated injury | Granular IgG IgG The major immunoglobulin isotype class in normal human serum. There are several isotype subclasses of igg, for example, igg1, igg2a, and igg2b. Hypersensitivity Pneumonitis, other Igs Igs Immunoglobulins (Igs), also known as antibodies, are glycoprotein molecules produced by plasma cells that act in immune responses by recognizing and binding particular antigens. The various ig classes are IgG (the most abundant), IgM, IgE, IgD, and IgA, which differ in their biologic features, structure, target specificity, and distribution. Immunoglobulins: Types and Functions, and complement |
|
|
| Pauci-immune crescentic glomerulonephritis | No deposits |
|
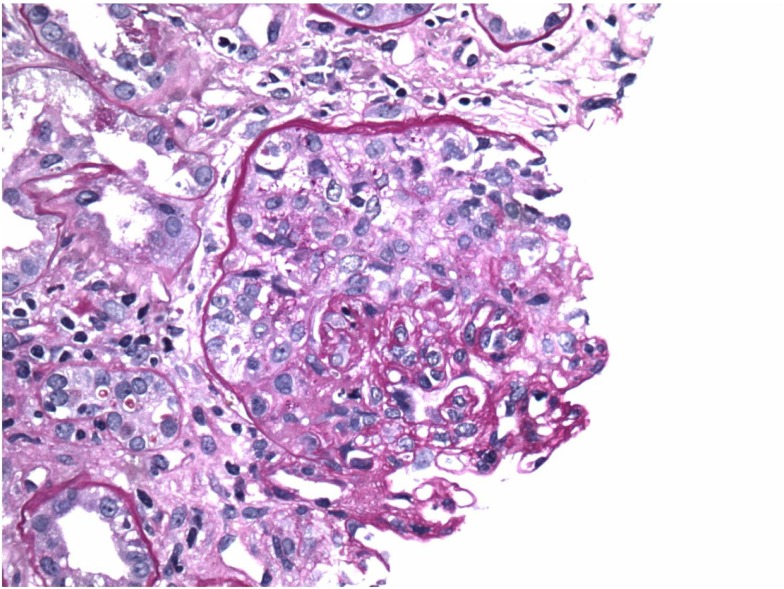
Anti-glomerular basement membrane (anti-GBM) antibody disease: crescents on light microscopy
Image: “Crescents on light microscopy” by Mavani G. P., Pommier M., Win S., Michelis M. F., Rosenstock J. License: CC BY 4.0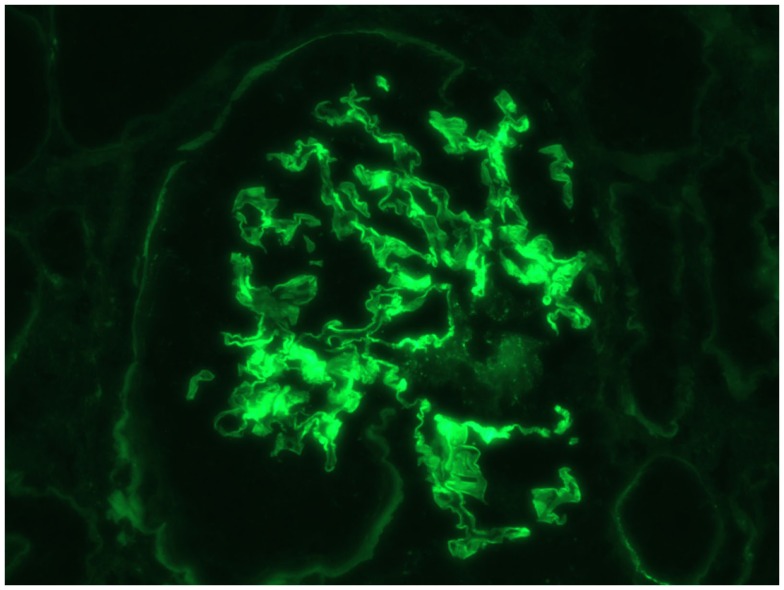
Anti-glomerular basement membrane (anti-GBM) antibody disease: IF linear staining of IgG
Image: “Immunofluorescence linear staining of IgG” by Mavani G. P., Pommier M., Win S., Michelis M. F., Rosenstock J. License: CC BY 4.0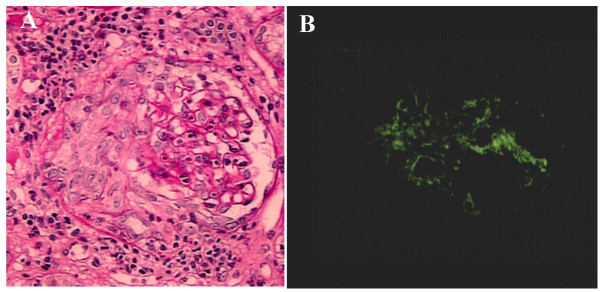
Infective endocarditis-induced rapidly progressive glomerulonephritis (RPGN) on PAS and IF:
A: PAS demonstrating circumferential and cellular crescent formation with interstitial nephritis
B: IF demonstrating C3-positive staining in the mesangial area
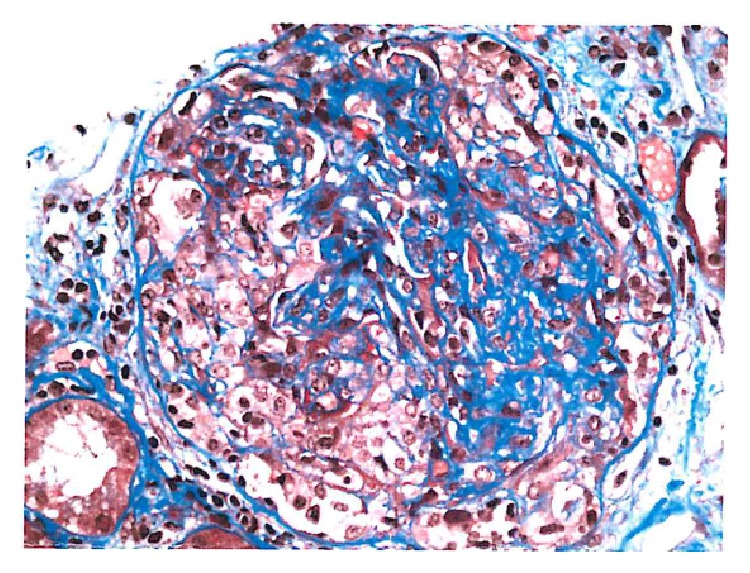
Pauci-immune crescentic glomerulonephritis showing fibrin within the cellular crescents
Image: “Cellular crescent” by Syed R., Rehman A., Valecha G., El-Sayegh S. License: CC BY 3.0