A pneumothorax is a life-threatening condition in which air collects in the pleural space Pleural space The thin serous membrane enveloping the lungs (lung) and lining the thoracic cavity. Pleura consist of two layers, the inner visceral pleura lying next to the pulmonary parenchyma and the outer parietal pleura. Between the two layers is the pleural cavity which contains a thin film of liquid. Pleuritis, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with a sudden onset of sharp chest pain Sharp Chest Pain Chest Pain, dyspnea Dyspnea Dyspnea is the subjective sensation of breathing discomfort. Dyspnea is a normal manifestation of heavy physical or psychological exertion, but also may be caused by underlying conditions (both pulmonary and extrapulmonary). Dyspnea, and diminished breath sounds on exam. Symptom severity depends on the degree of the collapsed lung. A large or tension pneumothorax can result in cardiopulmonary collapse. A diagnosis is made with imaging, though tension pneumothorax is a clinical diagnosis. Management is based on the size and stability of the patient, and can include needle decompression and chest tube ( thoracostomy Thoracostomy Surgical procedure involving the creation of an opening (stoma) into the chest cavity for drainage; used in the treatment of pleural effusion; pneumothorax; hemothorax; and empyema. Hemothorax) placement.
Last updated: Dec 15, 2025
As air enters the pleural space Pleural space The thin serous membrane enveloping the lungs (lung) and lining the thoracic cavity. Pleura consist of two layers, the inner visceral pleura lying next to the pulmonary parenchyma and the outer parietal pleura. Between the two layers is the pleural cavity which contains a thin film of liquid. Pleuritis, which normally has a negative pressure, the elastic Elastic Connective Tissue: Histology recoil Recoil Vessels can stretch and return to their original shape after receiving the stroke volume of blood ejected by the left ventricle during systole. Arteries: Histology in the lung tissues causes either a partial or full lung collapse.
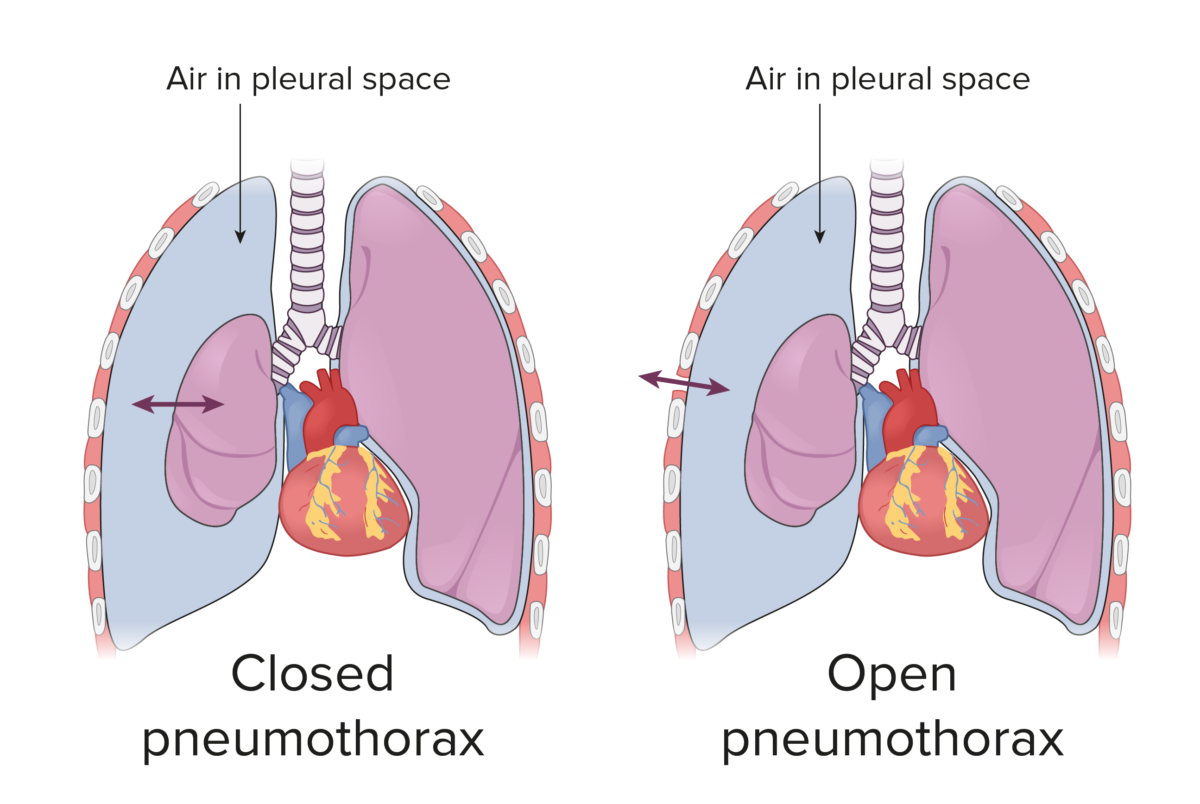
Closed and open pneumothoraces:
In a closed pneumothorax, air travels in and out of the pleural space from the lung. However, in an open pneumothorax, a defect in the chest wall allows air to move in and out of the pleural space.
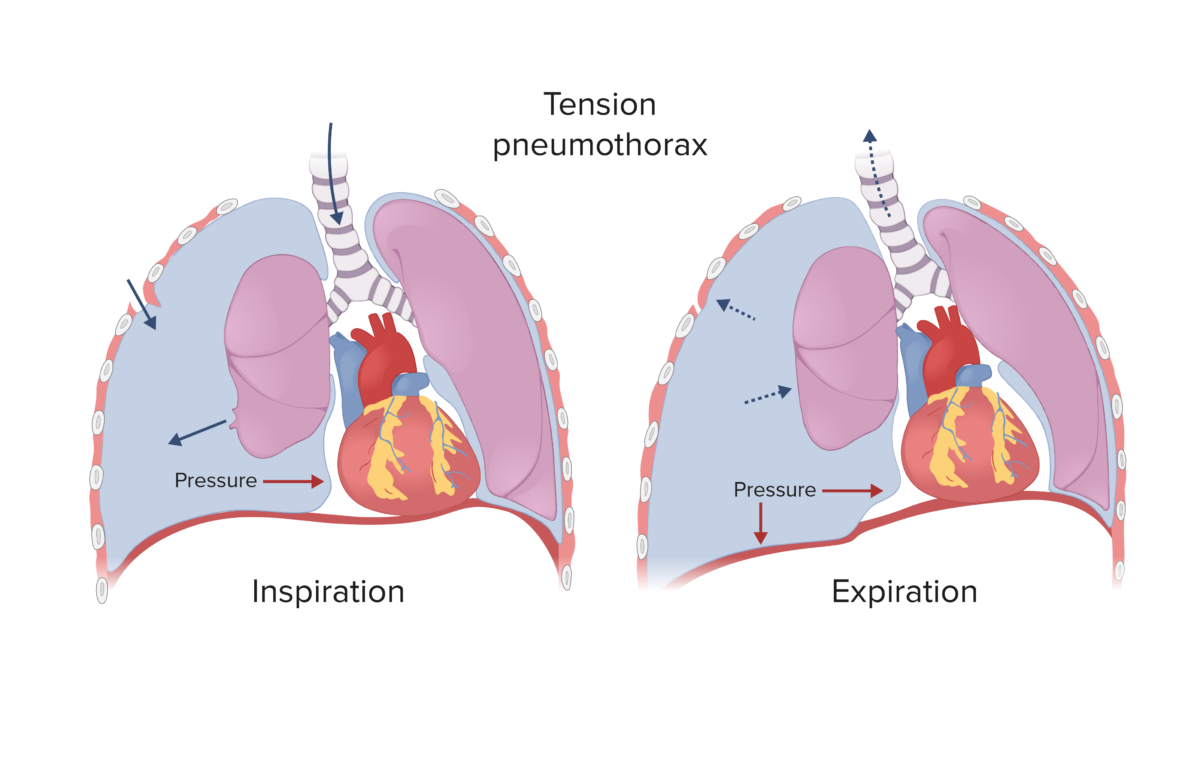
Tension pneumothorax:
Spontaneous and traumatic pneumothoraces can develop into a tension pneumothorax if the defect that allows air into the pleural space becomes a 1-way valve (air enters during inspiration, but cannot escape during expiration), which causes rising pressure in the pleural cavity, shifting the mediastinum to the contralateral side.
The clinical presentation will depend on the size of the pneumothorax. A tension pneumothorax will be associated with rapid clinical deterioration.
The signs and symptoms of tension pneumothorax is summarized with: P-THORAX:
The diagnosis is suspected based on the clinical presentation, and confirmed by imaging. Tension pneumothorax is a clinical diagnosis, and management should not wait for imaging confirmation.

Spontaneous pneumothorax in a young man on a CT scan
Image: “Spontaneous pneumothorax” by Hellerhoff. License: CC BY-SA 3.0.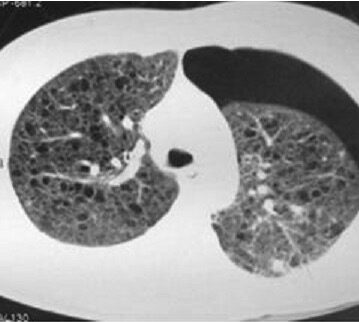
A CT showing a left-sided pneumothorax with multiple, bilateral, thin-walled cystic lesions replacing lung parenchyma in a patient with lymphangioleiomyomatosis
Image: “Left-sided pneumothorax” by the Department of Radiodiagnosis, Dayanand Medical College and Hospital, Ludhiana, Punjab, India. License: CC BY 2.0.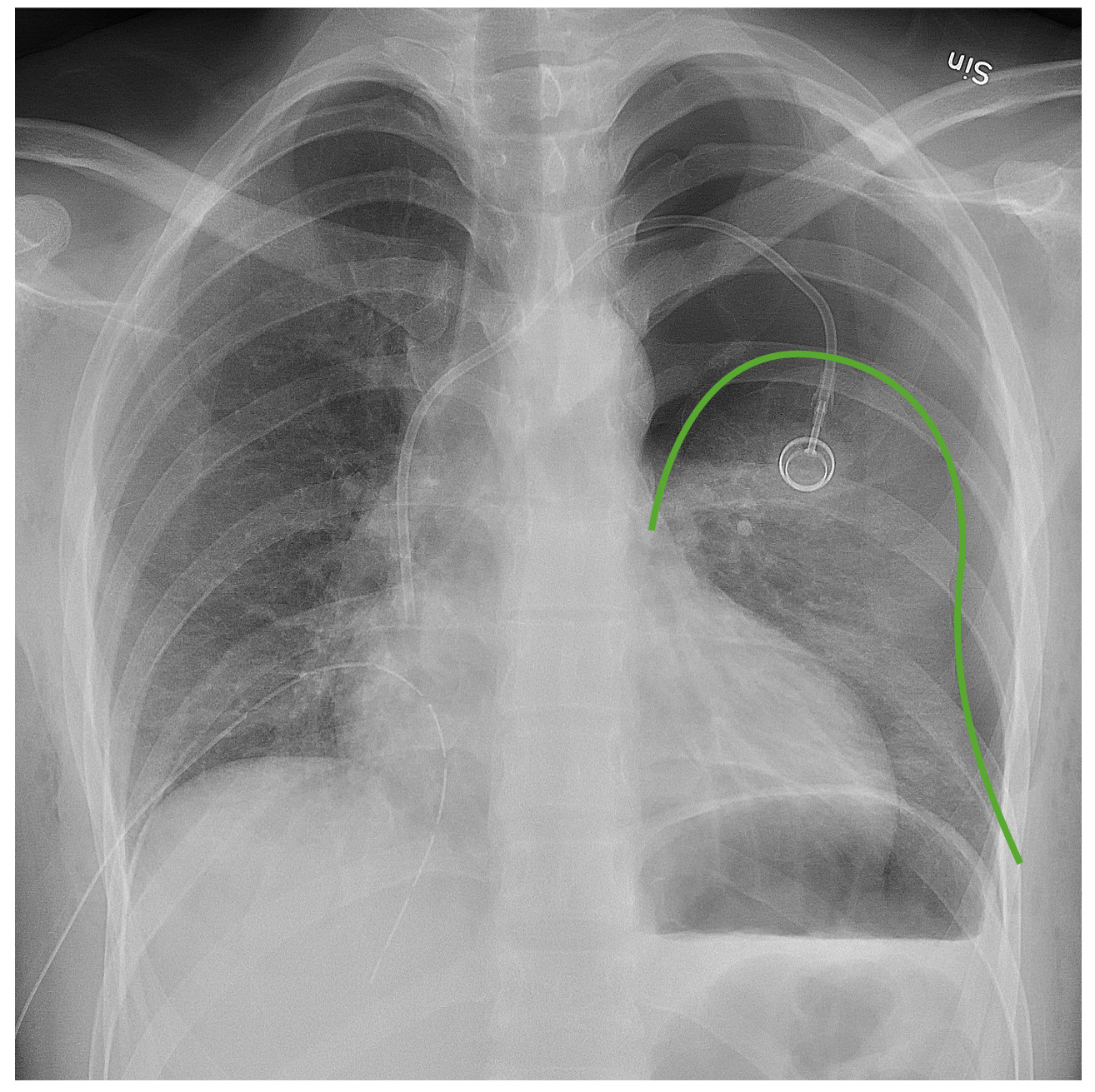
Chest radiograph demonstrating a left pneumothorax:
The green line outlines the pleural line. Notice the lack of bronchovascular markings beyond that line.
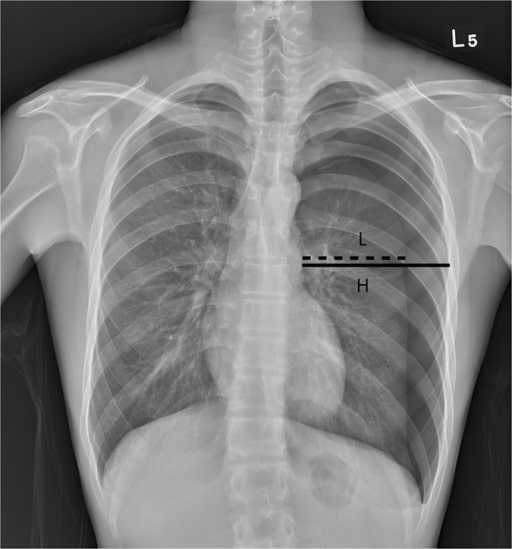
Chest radiograph of a patient with a left-sided pneumothorax:
H represents the diameter of the inner hemithorax at the hilar level, and L represents the diameter of the collapsed lung. The Light index, in this case, estimated the pneumothorax size to be 34%.
The management of a pneumothorax depends on the amount of air collected in the pleural cavity Pleural cavity Paired but separate cavity within the thoracic cavity. It consists of the space between the parietal and visceral pleura and normally contains a capillary layer of serous fluid that lubricates the pleural surfaces. Pleura: Anatomy and the stability of the patient.
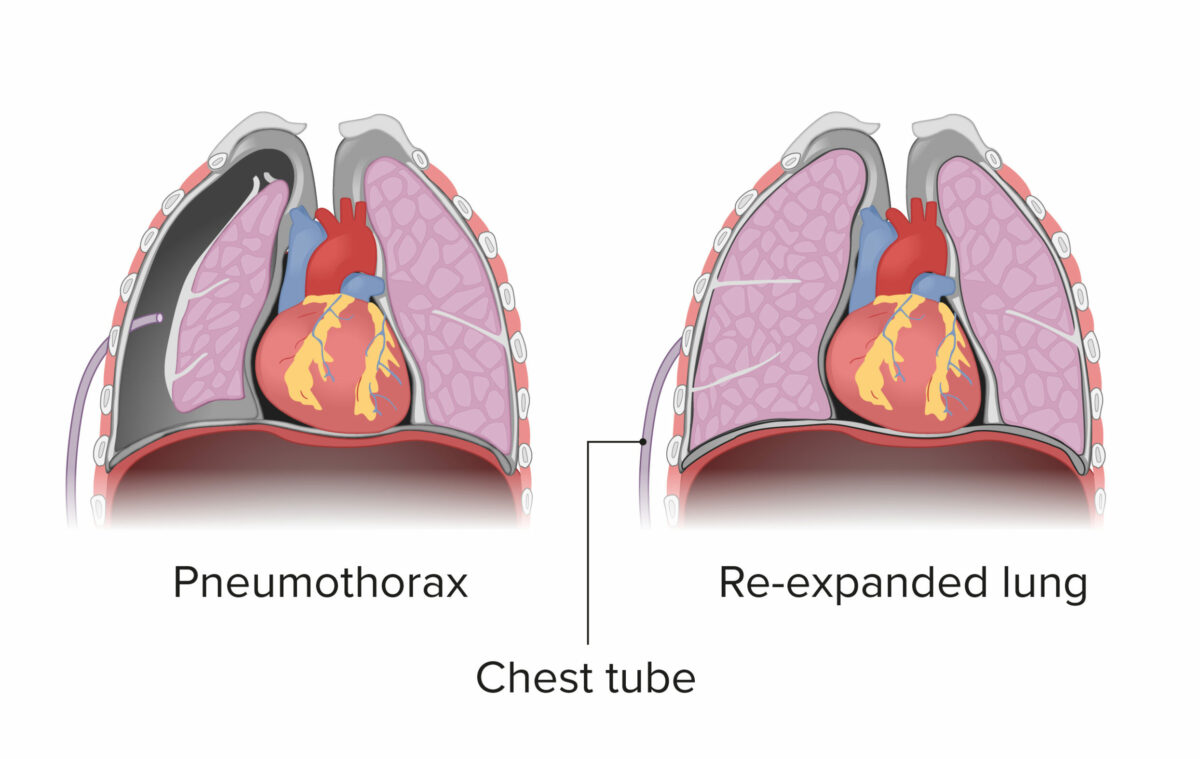
Demonstration of chest tube placement for a pneumothorax:
The chest tube is placed in the pleural space, which allows re-expansion of the collapsed lung.
Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are deemed stable if:
Small pneumothorax:
Large pneumothorax:
Definitive management: