Advertisement
Advertisement
Advertisement
Advertisement
Peripheral artery disease (PAD) is obstruction of the arterial lumen resulting in decreased blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure to the distal limbs. The disease can be a result of atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis or thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may be asymptomatic or have progressive claudication, skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions discoloration, ischemic ulcers, or gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction. Onset may be insidious ( atherosclerosis Atherosclerosis Atherosclerosis is a common form of arterial disease in which lipid deposition forms a plaque in the blood vessel walls. Atherosclerosis is an incurable disease, for which there are clearly defined risk factors that often can be reduced through a change in lifestyle and behavior of the patient. Atherosclerosis) or abrupt ( thrombosis Thrombosis Formation and development of a thrombus or blood clot in the blood vessel. Epidemic Typhus). Diagnosis is made with the clinical history, exam, and measurement of the ankle-brachial index Ankle-brachial index Comparison of the blood pressure between the brachial artery and the posterior tibial artery. It is a predictor of peripheral arterial disease. Cardiovascular Examination. Imaging studies can determine the location and extent of the arterial disease. Treatment varies depending on the severity but can include lifestyle modifications, antiplatelet therapy, risk factor modifications, phosphodiesterase inhibitors Phosphodiesterase inhibitors Phosphodiesterase (PDE) inhibitors are a group of drugs that act by inhibiting PDE enzymes. Phosphodiesterase inhibitors have various mechanisms of action depending on the subtype of PDE targeted, but their main action is increasing the amount of intracellular cAMP or cGMP, which in turn results in physiologic effects such as reducing inflammation, promoting smooth muscle relaxation, and vasodilation. Phosphodiesterase Inhibitors, and revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease).
Last updated: Nov 30, 2024
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Peripheral artery disease (PAD) usually has the same causative factors as coronary and carotid disease.
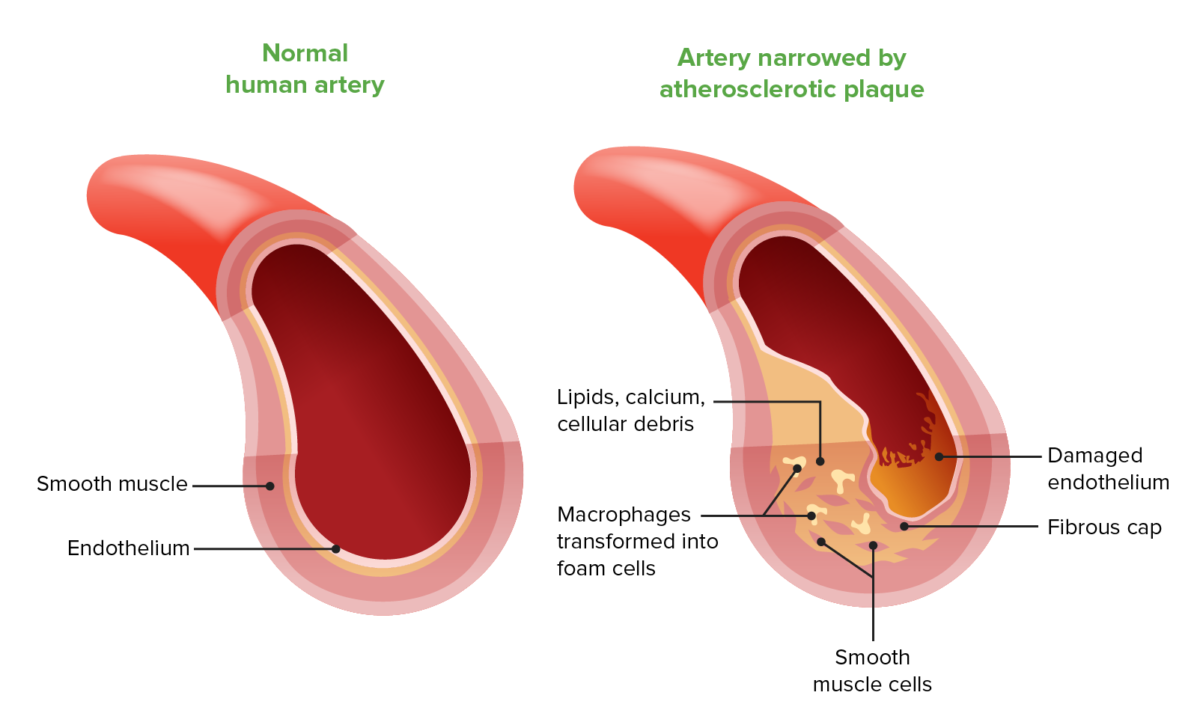
Composition of the fibrous plaque in atherosclerosis
Image by Lecturio.Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with PAD may be asymptomatic (20%–25%) or present with evidence of chronic or acute limb ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage.
| Stage | Symptoms |
|---|---|
| 1 | Asymptomatic |
| 2a | Intermittent claudication Intermittent claudication A symptom complex characterized by pain and weakness in skeletal muscle group associated with exercise, such as leg pain and weakness brought on by walking. Such muscle limpness disappears after a brief rest and is often relates to arterial stenosis; muscle ischemia; and accumulation of lactate. Thromboangiitis Obliterans (Buerger’s Disease) after walking > 200 meters (219 yards) |
| 2b | Intermittent claudication Intermittent claudication A symptom complex characterized by pain and weakness in skeletal muscle group associated with exercise, such as leg pain and weakness brought on by walking. Such muscle limpness disappears after a brief rest and is often relates to arterial stenosis; muscle ischemia; and accumulation of lactate. Thromboangiitis Obliterans (Buerger’s Disease) after walking < 200 meters (219 yards) |
| 3 | Nocturnal or resting pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways |
| 4 | Necrosis Necrosis The death of cells in an organ or tissue due to disease, injury or failure of the blood supply. Ischemic Cell Damage or gangrene Gangrene Death and putrefaction of tissue usually due to a loss of blood supply. Small Bowel Obstruction of the limb |
| Stage | Grade | Clinical Description | Objective Criteria |
|---|---|---|---|
| 0 | 0 | Asymptomatic | Normal treadmill/stress test |
| I | 1 | Mild claudication | Completes treadmill test; AP after exercise > 50 mmHg but at least 20 mmHg lower than resting |
| I | 2 | Moderate claudication | Between categories 1 and 3 |
| I | 3 | Severe claudication | Cannot complete standard treadmill test; AP after exercise < 50 mmHg |
| II | 4 | Ischemic rest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways | Resting AP < 40 mmHg, ankle/metatarsal PVR flat or barely pulsatile; TP < 30 mmHg |
| III | 5 | Minor tissue loss (non-healing ulcers, focal areas of poor blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure) | Resting AP < 60 mmHg, ankle/metatarsal PVR flat or barely pulsatile; TP < 40 mmHg |
| IV | 6 | Major tissue loss (damage extends above TM Tm Tubular System level, non-salvageable foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy) | Same as category 5 |

Bilateral cyanotic toes
Image: “Bilateral toes showing cyanosis” by Department of Anaesthesia and Intensive Care, Bhubaneswar, India. License: CC BY 2.0Any 1 of the following indicates that blood flow Blood flow Blood flow refers to the movement of a certain volume of blood through the vasculature over a given unit of time (e.g., mL per minute). Vascular Resistance, Flow, and Mean Arterial Pressure no longer meets the metabolic demands of the limb tissues at rest:

Non-healing arterial ulcer on the dorsum of the foot in a patient with PAD
Image: “Severe peripheral arterial disease” by Jonathan Moore. License: CC BY 3.0
Peripheral arterial disease resulting in necrosis of multiple toes
Image: “Peripheral arterial disease” by Karl-Christian Münter. License: CC BY 4.0Acute limb ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage is most commonly due to an embolism or plaque Plaque Primary Skin Lesions rupture. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will demonstrate acute onset of:
This algorithm demonstrates the diagnostic pathway for a patient presenting with signs or symptoms of PAD:
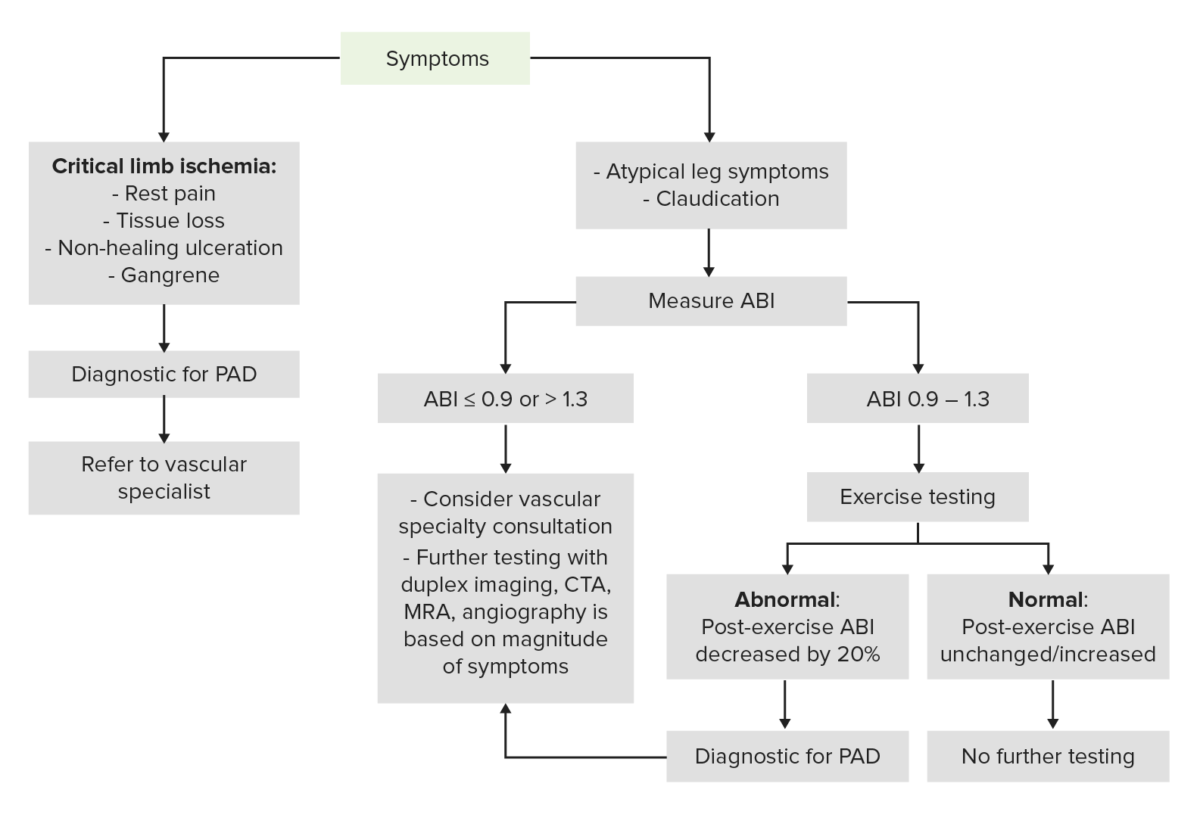
Diagnostic algorithm for PAD
Image by Lecturio.The diagnosis is usually established through clinical history, exam, and non-invasive testing techniques ( ankle-brachial index Ankle-brachial index Comparison of the blood pressure between the brachial artery and the posterior tibial artery. It is a predictor of peripheral arterial disease. Cardiovascular Examination (ABI), exercise testing).
Note that those with features of limb-threatening ischemia Ischemia A hypoperfusion of the blood through an organ or tissue caused by a pathologic constriction or obstruction of its blood vessels, or an absence of blood circulation. Ischemic Cell Damage need urgent vascular surgery Vascular surgery Vascular surgery is the specialized field of medicine that focuses on the surgical management of the pathologies of the peripheral circulation. The main goal of most vascular procedures is to restore circulatory function to the affected vessels by relieving occlusions or by redirecting blood flow (e.g., bypass). Vascular Surgery evaluation. These patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship may still undergo imaging studies to locate the area of vascular obstruction or stenosis Stenosis Hypoplastic Left Heart Syndrome (HLHS) as part of surgical planning.
These studies are used to establish the diagnosis:
| Parameter | Value |
|---|---|
| Normal | ≥ 0.9 |
| Mild | 0.71–0.9 |
| Moderate | 0.41–0.7 |
| Severe | ≤ 0.4 |
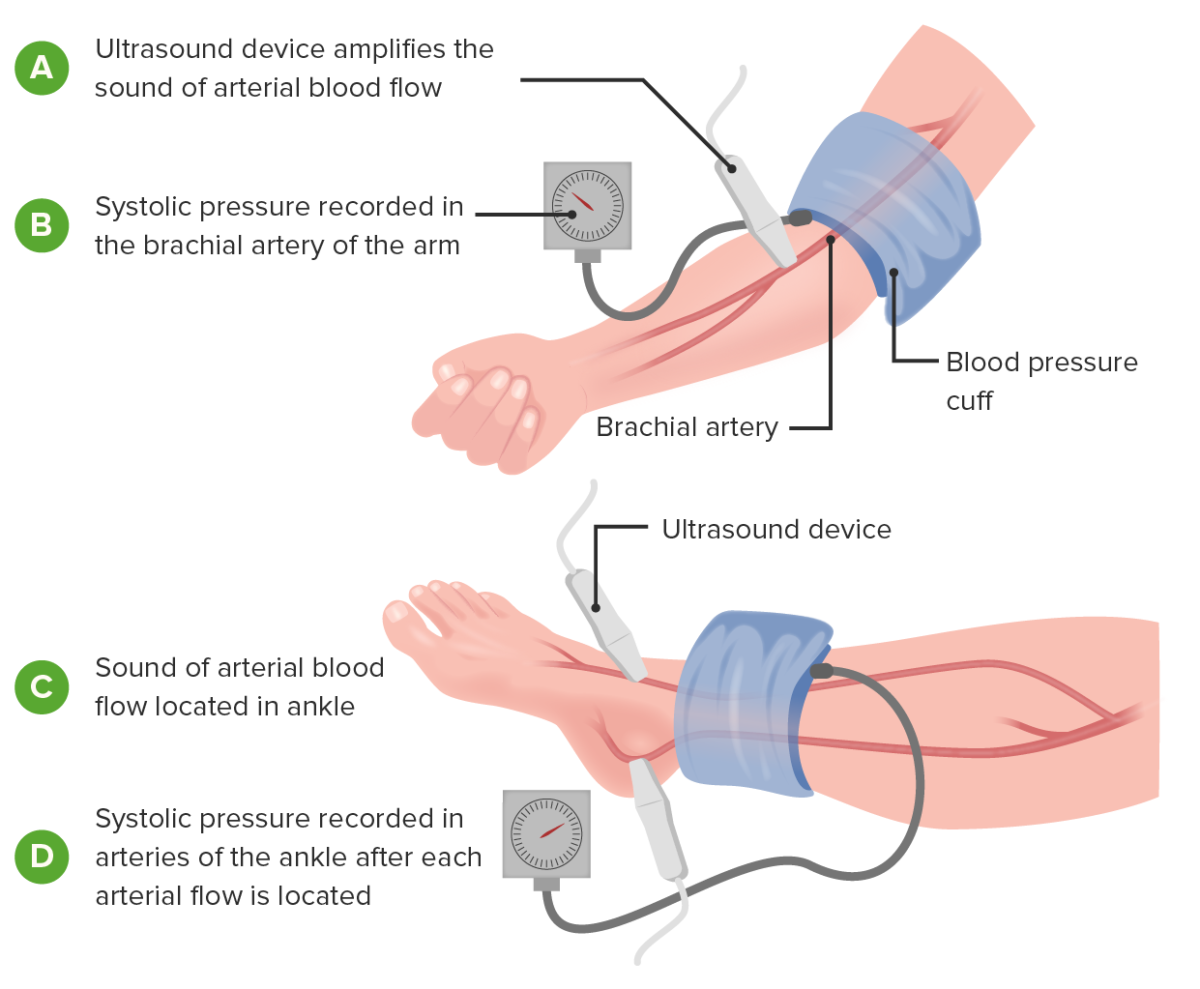
Image demonstrating how to measure the ankle-brachial index: This assists in the diagnosis and severity determination of PAD.
Image by Lecturio.These studies are used to evaluate the location and severity of disease:
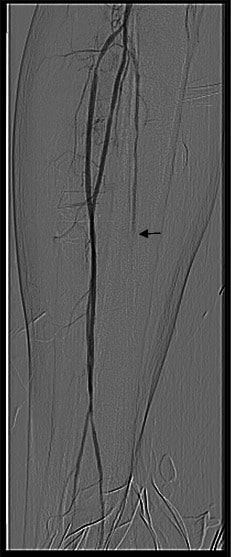
Arteriography showing occlusion of the posterior tibial artery (arrow)
Image: “Posterior tibial artery occlusion” by C. Voiculeț et al. License: CC BY 2.0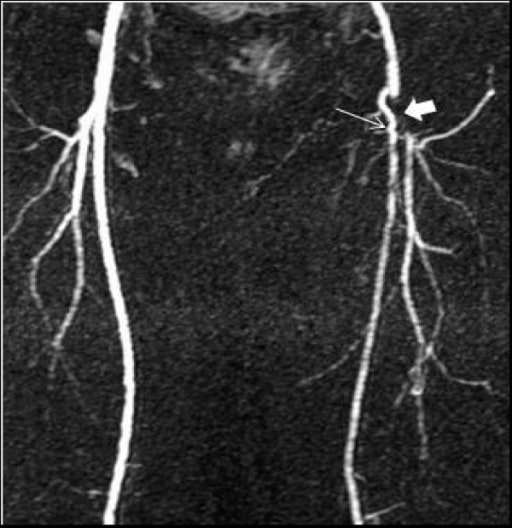
An MRA demonstrating occluded left distal common and proximal superficial (thin arrow) and profunda (thick arrow) femoral arteries, with a collateral artery connecting the 2
Image: “F1” by Bariatric and Metabolic Institute & Dept. of Surgery, Cleveland Clinic, 9500 Euclid Avenue, Cleveland 44950, Ohio, USA. License: CC BY 2.0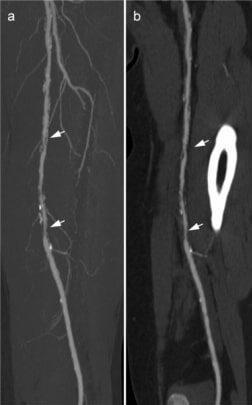
These CTA images demonstrate stenosis (arrows) in the left superficial femoral artery.
Image: “Example of a run-off CTA” by Klinik für Radiologie, Charité Universitätsmedizin Berlin, Berlin, Germany. License: CC BY 4.0These studies are not used for the diagnosis of PAD, but can help evaluate risk factors or organ injury:
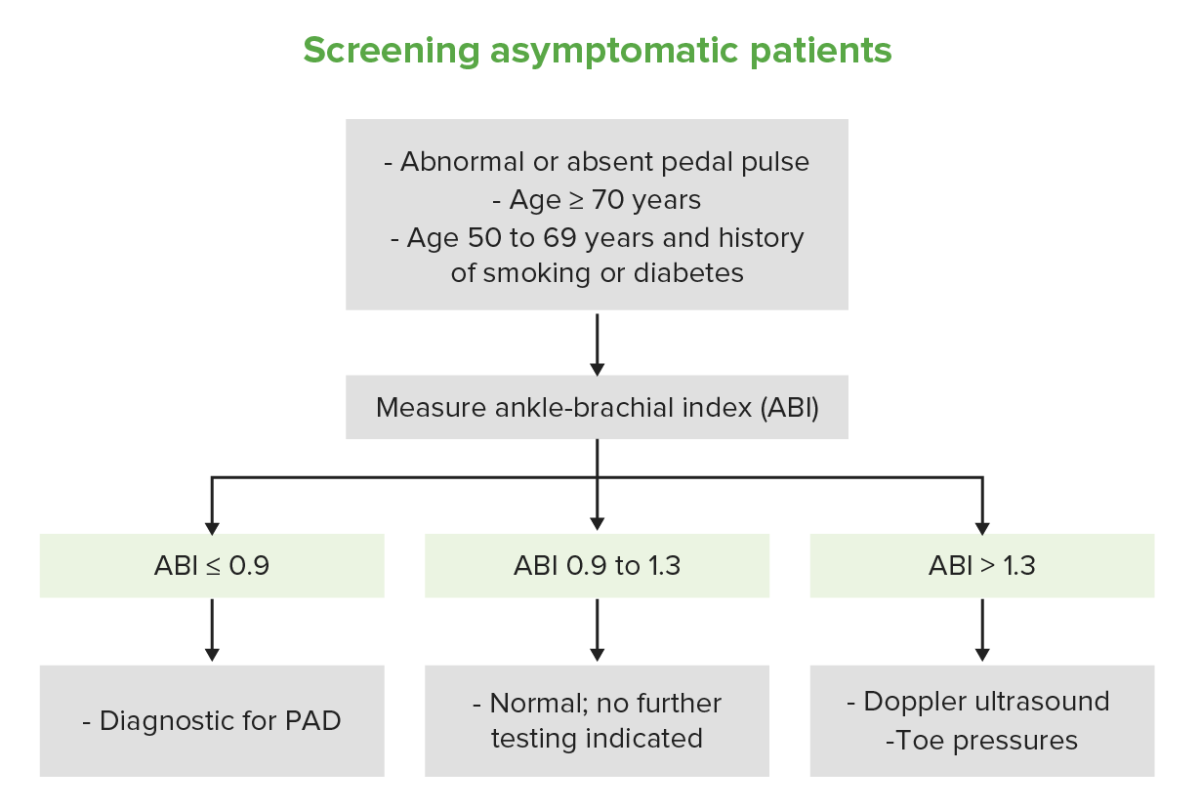
Screening asymptomatic patients
Image by Lecturio.Lifestyle modification is the 1st line of therapy:
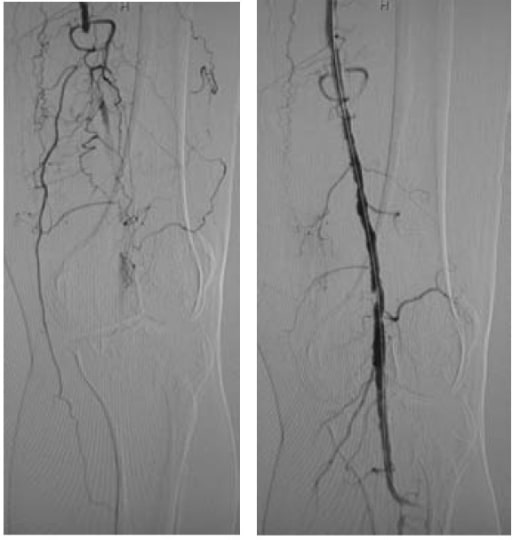
Left: left popliteal artery occlusion
Right: return of blood flow after PTA with stenting
Amputation Amputation An amputation is the separation of a portion of the limb or the entire limb from the body, along with the bone. Amputations are generally indicated for conditions that compromise the viability of the limb or promote the spread of a local process that could manifest systemically. Amputation is performed when:
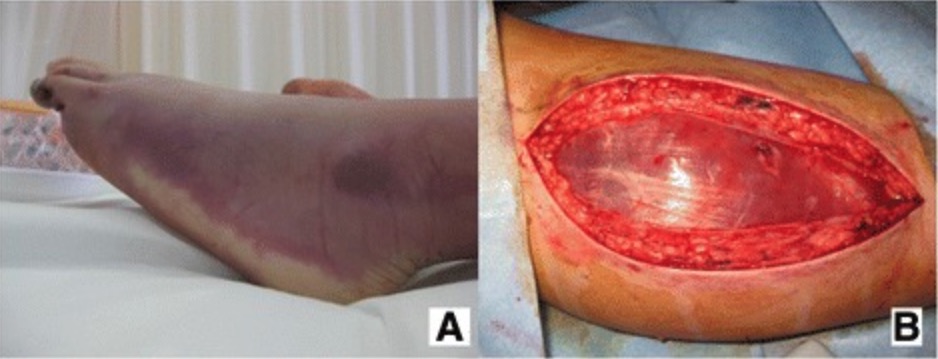
Images demonstrating an ischemic limb (A) that developed compartment syndrome: A fasciotomy (B) was required.
Image: “Fig1” by Yohei Okada. License: CC BY 4.0