Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea is described as passage of large amounts stools that are often loose, liquid, or watery, resulting in excess loss of fluids and electrolytes Electrolytes Electrolytes are mineral salts that dissolve in water and dissociate into charged particles called ions, which can be either be positively (cations) or negatively (anions) charged. Electrolytes are distributed in the extracellular and intracellular compartments in different concentrations. Electrolytes are essential for various basic life-sustaining functions. Electrolytes. Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea is one of the most common illnesses in children, representing the largest percentages of morbidity Morbidity The proportion of patients with a particular disease during a given year per given unit of population. Measures of Health Status and mortality Mortality All deaths reported in a given population. Measures of Health Status worldwide in the pediatric age group. The majority of cases are infectious, caused by rotavirus Rotavirus A genus of Reoviridae, causing acute gastroenteritis in birds and mammals, including humans. Transmission is horizontal and by environmental contamination. Seven species (rotaviruses A through G) are recognized. Rotavirus, while the rest are caused by bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology ( Escherichia coli Escherichia coli The gram-negative bacterium Escherichia coli is a key component of the human gut microbiota. Most strains of E. coli are avirulent, but occasionally they escape the GI tract, infecting the urinary tract and other sites. Less common strains of E. coli are able to cause disease within the GI tract, most commonly presenting as abdominal pain and diarrhea. Escherichia coli, Salmonella Salmonella Salmonellae are gram-negative bacilli of the family Enterobacteriaceae. Salmonellae are flagellated, non-lactose-fermenting, and hydrogen sulfide-producing microbes. Salmonella enterica, the most common disease-causing species in humans, is further classified based on serotype as typhoidal (S. typhi and paratyphi) and nontyphoidal (S. enteritidis and typhimurium). Salmonella) and parasites ( Entamoeba histolytica Entamoeba Histolytica A species of parasitic protozoa causing entamoebiasis and amebic dysentery (dysentery, amebic). Characteristics include a single nucleus containing a small central karyosome and peripheral chromatin that is finely and regularly beaded. Amebicides). Management is largely based on rehydration Rehydration Dengue Virus; antibiotic therapy is used only when indicated. Prognosis Prognosis A prediction of the probable outcome of a disease based on a individual's condition and the usual course of the disease as seen in similar situations. Non-Hodgkin Lymphomas is excellent if diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea promptly treated.
Last updated: Dec 15, 2025
Diarrhea Diarrhea Diarrhea is defined as ≥ 3 watery or loose stools in a 24-hour period. There are a multitude of etiologies, which can be classified based on the underlying mechanism of disease. The duration of symptoms (acute or chronic) and characteristics of the stools (e.g., watery, bloody, steatorrheic, mucoid) can help guide further diagnostic evaluation. Diarrhea is defined as excess stool output that is often loose or watery.
Quantification of stool output varies:
Infants and young children:
Older children:
Infants and young children:
Older children:
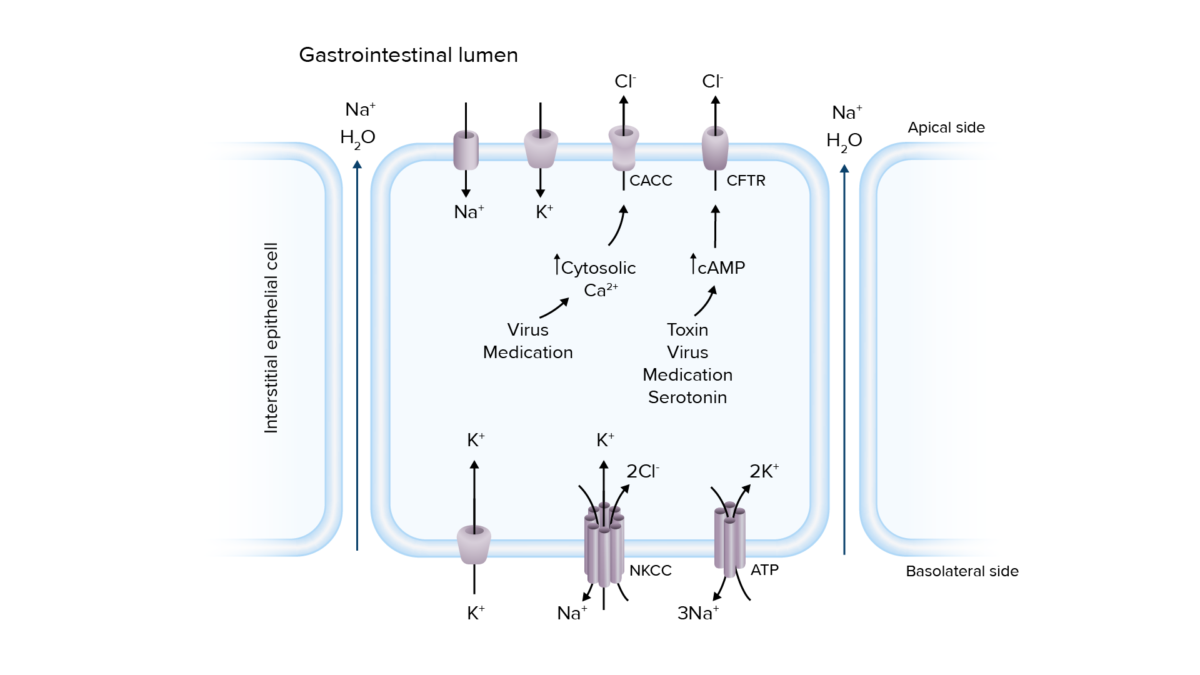
Pathogenesis of secretory diarrhea:
Overactivation of ion transport channels can lead to secretion of electrolytes and water into the intestinal lumen, resulting in diarrhea.
Ca2+: calcium
CaCC: calcium-activated chloride channels
cAMP: cyclic adenosine monophosphate
CFTR: cystic fibrosis transmembrane conductance regulator
Cl−: chloride
K+: potassium
Na+: sodium
NKCC: sodium–potassium chloride cotransporter
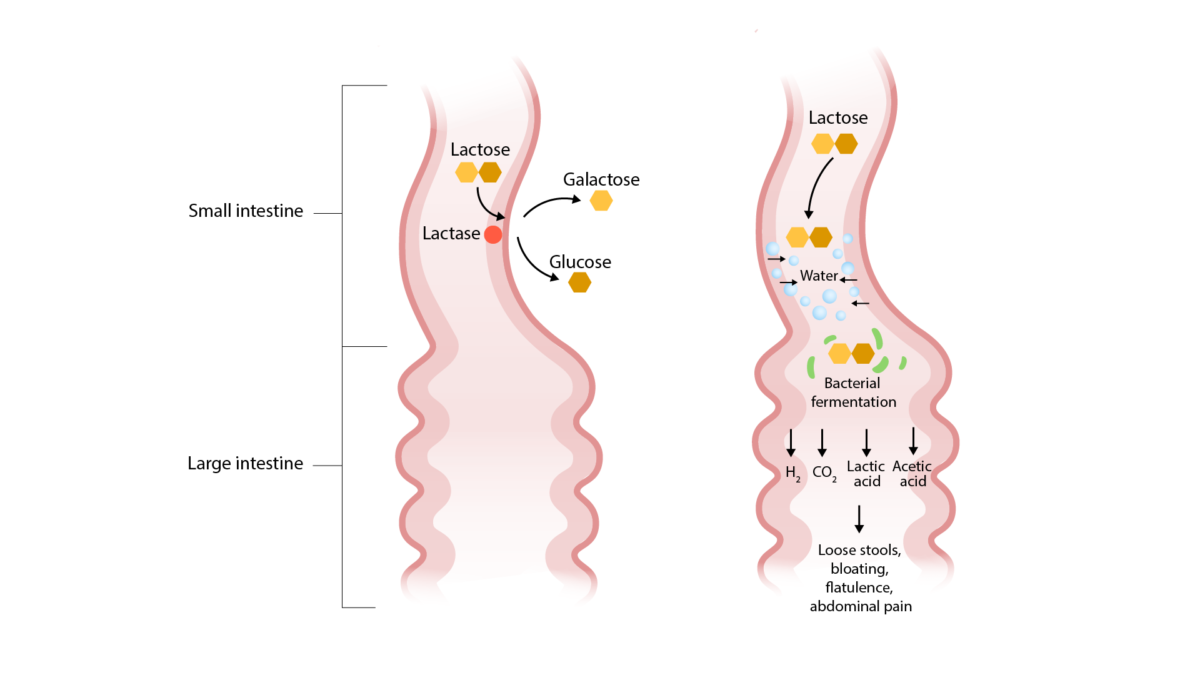
Pathogenesis of lactase deficiency (an etiology of osmotic diarrhea):
Lactose is not broken down and remains in the small intestinal lumen. This draws in water, causing osmotic diarrhea. Bacterial fermentation of lactose results in the symptoms of bloating, flatulence, and abdominal pain.
| Mild | Moderate | Severe | |
|---|---|---|---|
| Weight loss Weight loss Decrease in existing body weight. Bariatric Surgery |
|
|
|
| Dry mucosa (1st sign) | – | +/–, looks dry | +, looks parched |
| Skin turgor Skin turgor Malnutrition in children in resource-limited countries (last sign) | + | +/– | ++/+ |
| Anterior fontanelle depression Anterior fontanelle depression Malnutrition in children in resource-limited countries | – | + | ++/+ |
| Mental status | Normal | Fatigue Fatigue The state of weariness following a period of exertion, mental or physical, characterized by a decreased capacity for work and reduced efficiency to respond to stimuli. Fibromyalgia/irritability | Apathy Apathy Lack of emotion or emotional expression; a disorder of motivation that persists over time. Wernicke Encephalopathy and Korsakoff Syndrome/ lethargy Lethargy A general state of sluggishness, listless, or uninterested, with being tired, and having difficulty concentrating and doing simple tasks. It may be related to depression or drug addiction. Hyponatremia |
| Enophthalmos Enophthalmos Recession of the eyeball into the orbit. Marfan Syndrome | – | + | + |
| Breathing | Normal | Deep, may be tachypneic | Deep and tachypneic |
| HR | Normal | Increased | Very high |
| Hypotension Hypotension Hypotension is defined as low blood pressure, specifically < 90/60 mm Hg, and is most commonly a physiologic response. Hypotension may be mild, serious, or life threatening, depending on the cause. Hypotension | – | + | + |
| Distal perfusion | Normal |
|
|
| Urinary output | Decreased | Oliguria Oliguria Decreased urine output that is below the normal range. Oliguria can be defined as urine output of less than or equal to 0. 5 or 1 ml/kg/hr depending on the age. Renal Potassium Regulation | Oliguria Oliguria Decreased urine output that is below the normal range. Oliguria can be defined as urine output of less than or equal to 0. 5 or 1 ml/kg/hr depending on the age. Renal Potassium Regulation/ anuria Anuria Absence of urine formation. It is usually associated with complete bilateral ureteral (ureter) obstruction, complete lower urinary tract obstruction, or unilateral ureteral obstruction when a solitary kidney is present. Acute Kidney Injury |
Workup is generally not needed and is indicated only in cases of moderate to severe dehydration Severe Dehydration Fluid Replacement Therapy in Children, immunocompromise, and sepsis Sepsis Systemic inflammatory response syndrome with a proven or suspected infectious etiology. When sepsis is associated with organ dysfunction distant from the site of infection, it is called severe sepsis. When sepsis is accompanied by hypotension despite adequate fluid infusion, it is called septic shock. Sepsis and Septic Shock and in chronic cases.
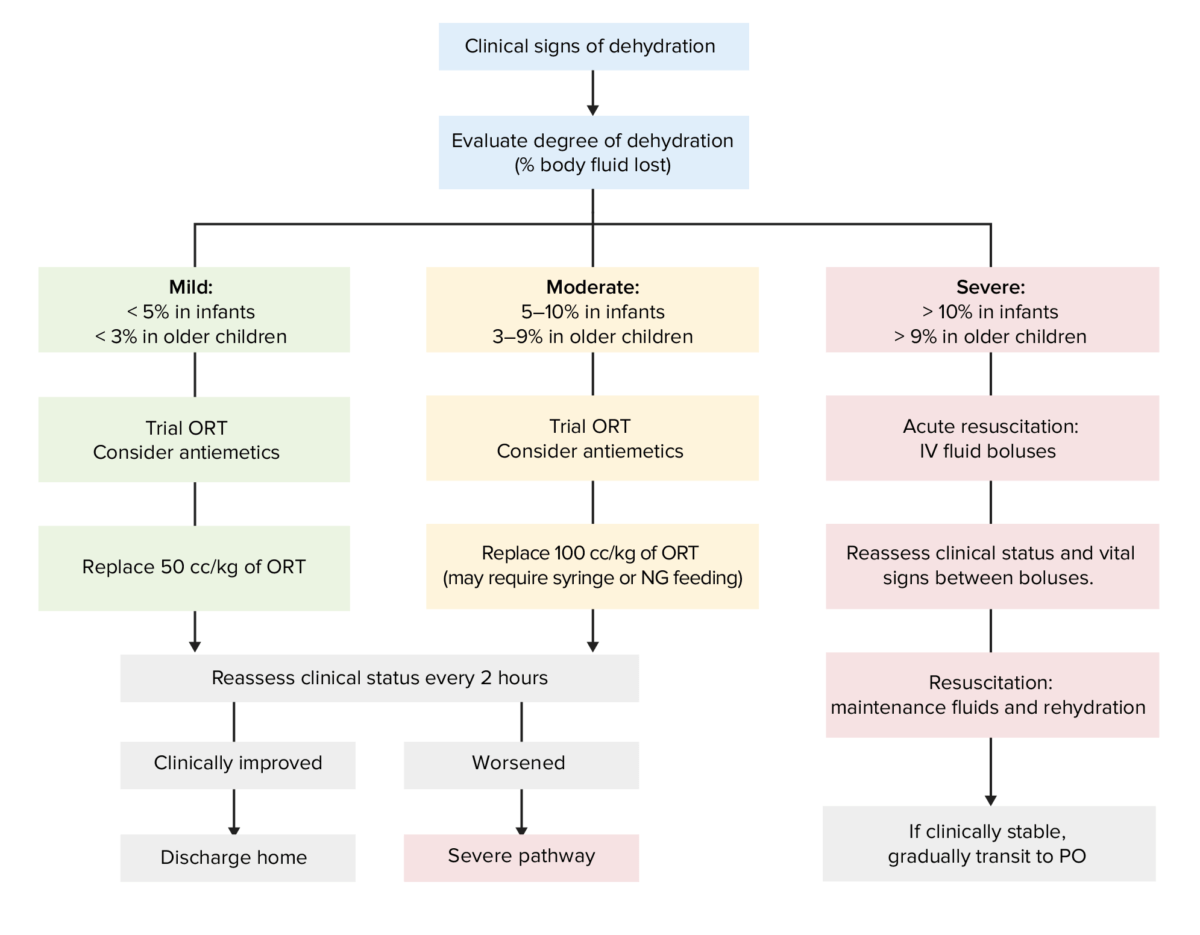
Flowchart for the evaluation and treatment of dehydration based on the severity of symptoms
ORT: oral replacement therapy
PO: per os (used to indicated oral intake/administration)
NG: nasogastric