Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus, but a variety of organisms have been linked to osteomyelitis. The majority of patients present with pain, redness, and swelling of the affected site, and may have associated symptoms such as fever and chills. Laboratory values will demonstrate elevated WBC, CRP, and erythrocyte sedimentation rate (ESR) in most cases. The most sensitive and specific imaging modality to diagnose osteomyelitis is MRI. Management may require long-term antibiotics and potential surgical debridement.
Last updated: Dec 15, 2025
Osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis is classified based on the route of infection.
Non-hematogenous osteomyelitis Non-hematogenous osteomyelitis Osteomyelitis resulting from direct inoculation of bacteria due to surgery, prosthetic devices, trauma, hardware for fracture fixation, soft tissue infection. Osteomyelitis (80% of cases):
Hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis (20% of cases):
| Risk factors | Infectious agents |
|---|---|
| No specific risk factor | S. aureus S. aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Staphylococcus |
| Prosthetic joint replacement Prosthetic Joint Replacement Septic Arthritis |
|
| Sickle cell anemia Sickle cell anemia A disease characterized by chronic hemolytic anemia, episodic painful crises, and pathologic involvement of many organs. It is the clinical expression of homozygosity for hemoglobin S. Sickle Cell Disease |
|
| Chronic granulomatous disease Granulomatous disease A defect of leukocyte function in which phagocytic cells ingest but fail to digest bacteria, resulting in recurring bacterial infections with granuloma formation. When chronic granulomatous disease is caused by mutations in the cybb gene, the condition is inherited in an X-linked recessive pattern. When chronic granulomatous disease is caused by cyba, ncf1, ncf2, or ncf4 gene mutations, the condition is inherited in an autosomal recessive pattern. Common Variable Immunodeficiency (CVID) |
|
| Vertebral osteomyelitis Vertebral Osteomyelitis Osteomyelitis |
|
| Sexually active, no other risk factors | N. gonorrhoeae N. gonorrhoeae A species of gram-negative, aerobic bacteria primarily found in purulent venereal discharges. It is the causative agent of gonorrhea. Neisseria (more likely to cause septic arthritis Arthritis Acute or chronic inflammation of joints. Osteoarthritis than osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis) |
| Cat or dog bite | Pasteurella multocida Pasteurella Multocida A species of gram-negative, facultatively anaerobic, rod-shaped bacteria normally found in the flora of the mouth and respiratory tract of animals and birds. It causes shipping fever; hemorrhagic bacteremia; and intestinal disease in animals. In humans, disease usually arises from a wound infection following a bite or scratch from domesticated animals. Dog and Cat Bites |
| IV drug use or immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis |
|
Osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis is an infection of the bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types that results from hematogenous Hematogenous Hepatocellular Carcinoma (HCC) and Liver Metastases or non-hematogenous spread of infectious organisms.[1,3,7–11]
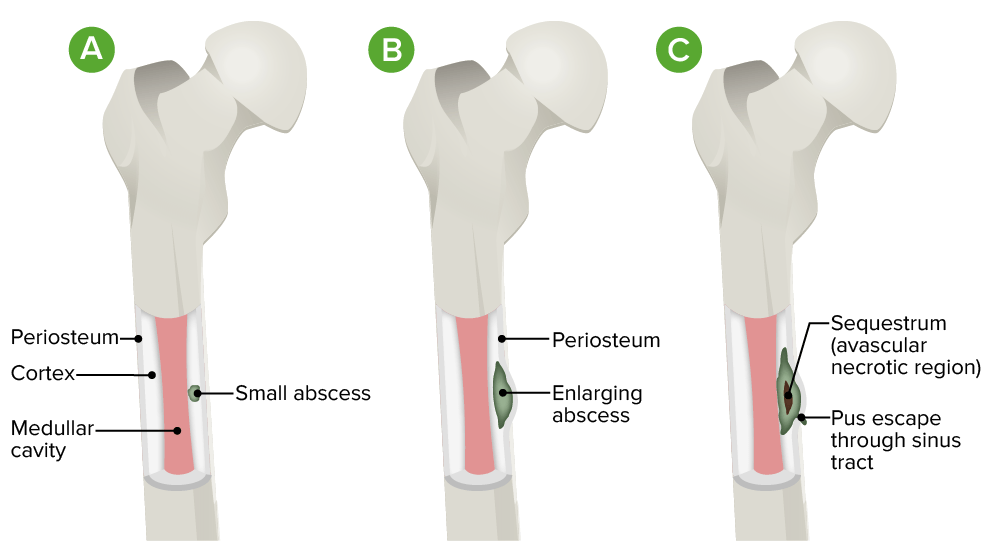
Pathophysiology of osteomyelitis:
A. Initial infection is localized to the cortical region.
B. There is progression into the subperiosteal space with lifting of the periosteum.
C. Diffuse infection occurs with sequestrum (avascular necrotic region) and sinus tract formation.
Vertebral osteomyelitis Vertebral Osteomyelitis Osteomyelitis:
Sternoclavicular and pelvic osteomyelitis Pelvic Osteomyelitis Osteomyelitis:
Long bone osteomyelitis Long Bone Osteomyelitis Osteomyelitis:

X-ray of the hand showing chronic osteomyelitis:
Note the bony destruction at the radiocarpal joint.

An MRI of the left foot with osseous changes of the calcaneus consistent with osteomyelitis
Image: “Delayed recognition of pediatric calcaneal osteomyelitis: a case report” by Mallia AJ, Ashwood N, Arealis G, Bindi F, Zamfir G, Galanopoulos I. License: CC BY 4.0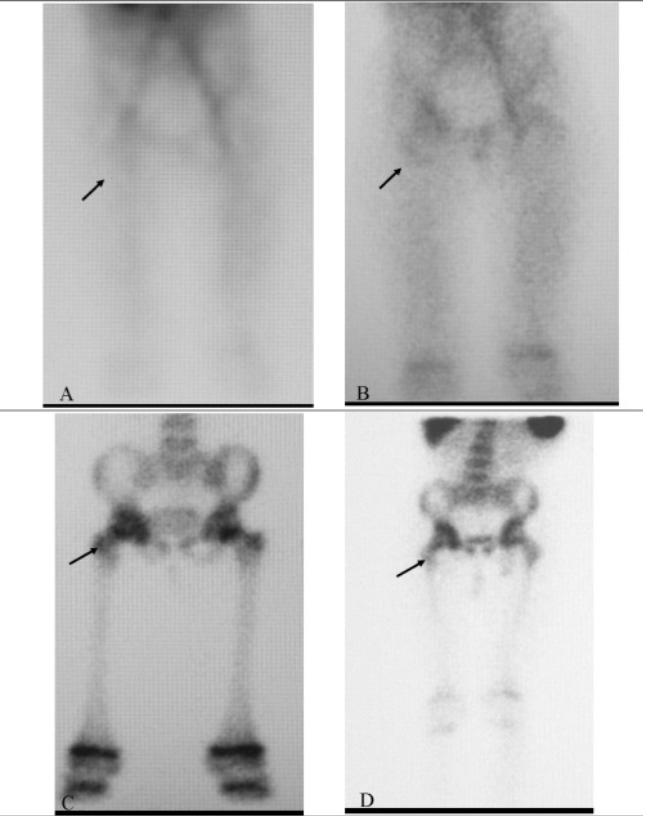
A 3-phase bone scan showing positive uptake in the region of the right hip (arrow) in a patient with osteomyelitis
Image: “Tc-99m Labeled HMPAO white Blood Cell Scintigraphy in Pediatric Patients” by Aydın F, Kın Cengiz A, Güngör F. License: CC BY 2.5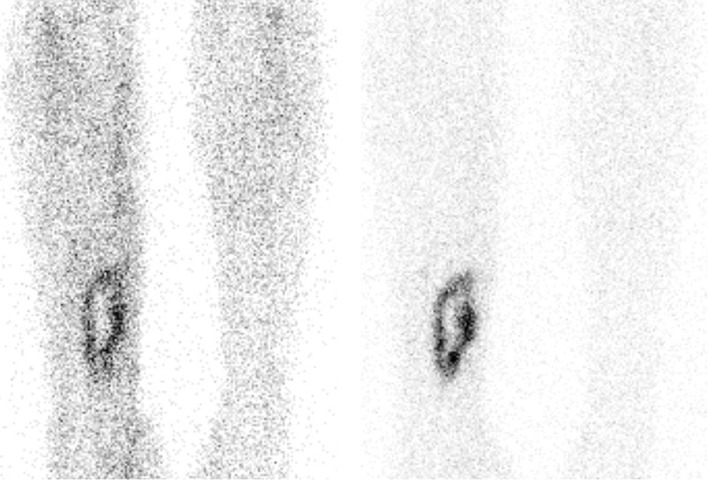
An example of a positive tagged WBC scan in a patient with osteomyelitis of the right tibia.
Increased uptake is seen in the right tibia, compared with the background uptake.
Left image: anterior view 4 hours after injection
Right image: anterior view 24 hours after injection.
Treatment of osteomyelitis Osteomyelitis Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus. Osteomyelitis involves antibiotic therapy and surgical debridement Debridement The removal of foreign material and devitalized or contaminated tissue from or adjacent to a traumatic or infected lesion until surrounding healthy tissue is exposed. Stevens-Johnson Syndrome of infected and necrotic tissue (with possible removal of infected hardware).
General considerations:
Options:
| Microorganism | Antibiotic options |
|---|---|
| Methicillin-sensitive Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess (MSSA) | |
| Methicillin-resistant Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess ( MRSA MRSA A strain of Staphylococcus aureus that is non-susceptible to the action of methicillin. The mechanism of resistance usually involves modification of normal or the presence of acquired penicillin binding proteins. Staphylococcus) | |
| Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus | |
| Enterococci | |
| Quinolone-sensitive Enterobacteriaceae Enterobacteriaceae A family of gram-negative, facultatively anaerobic, rod-shaped bacteria that do not form endospores. Its organisms are distributed worldwide with some being saprophytes and others being plant and animal parasites. Many species are of considerable economic importance due to their pathogenic effects on agriculture and livestock. Cephalosporins(gram-negative) | |
| Quinolone-resistant Enterobacteriaceae Enterobacteriaceae A family of gram-negative, facultatively anaerobic, rod-shaped bacteria that do not form endospores. Its organisms are distributed worldwide with some being saprophytes and others being plant and animal parasites. Many species are of considerable economic importance due to their pathogenic effects on agriculture and livestock. Cephalosporins (gram-negative) | |
| Pseudomonas aeruginosa Pseudomonas aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas |
Ciprofloxacin
Ciprofloxacin
A broad-spectrum antimicrobial carboxyfluoroquinoline.
Fluoroquinolones,
levofloxacin
Levofloxacin
The l-isomer of ofloxacin.
Fluoroquinolones,
cefepime
Cefepime
A fourth-generation cephalosporin antibacterial agent that is used in the treatment of infections, including those of the abdomen, urinary tract, respiratory tract, and skin. It is effective against pseudomonas aeruginosa and may also be used in the empiric treatment of febrile neutropenia.
Cephalosporins,
ceftazidime
Ceftazidime
Semisynthetic, broad-spectrum antibacterial derived from cephaloridine and used especially for pseudomonas and other gram-negative infections in debilitated patients.
Cephalosporins, and
meropenem
Meropenem
A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients.
Carbapenems and Aztreonam have antipseudomonal activity (see antibiotic dosing in the antibiotics for gram-negative organisms above). Other recommendations: |
| Anaerobes Anaerobes Lincosamides |
Indications:
Surgical principles:
Diagnosis Codes:
These codes are used to diagnose
osteomyelitis
Osteomyelitis
Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus.
Osteomyelitis, an infection of the
bone
Bone
Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy.
Bones: Structure and Types. The codes specify acuity (acute vs. chronic) and the affected site.
| Coding System | Code | Description |
|---|---|---|
| ICD-10-CM | M86.10 | Other acute osteomyelitis Acute osteomyelitis Osteomyelitis evolves over days or weeks. Osteomyelitis, unspecified site |
| ICD-10-CM | M86.671 | Other chronic osteomyelitis Chronic osteomyelitis Osteomyelitis persists over months to years and causes bone ischemia and necrosis, bone loss, sinus tract formation. Osteomyelitis, right ankle and foot Foot The foot is the terminal portion of the lower limb, whose primary function is to bear weight and facilitate locomotion. The foot comprises 26 bones, including the tarsal bones, metatarsal bones, and phalanges. The bones of the foot form longitudinal and transverse arches and are supported by various muscles, ligaments, and tendons. Foot: Anatomy |
Evaluation & Workup:
An MRI is the most sensitive imaging study for detecting early
osteomyelitis
Osteomyelitis
Osteomyelitis is an infection of the bone that results from the spread of microorganisms from the blood (hematogenous), nearby infected tissue, or open wounds (non-hematogenous). Infections are most commonly caused by Staphylococcus aureus.
Osteomyelitis. A
bone
Bone
Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy.
Bones: Structure and Types
biopsy
Biopsy
Removal and pathologic examination of specimens from the living body.
Ewing Sarcoma with culture is the definitive test to confirm the diagnosis and identify the causative organism.
| Coding System | Code | Description |
|---|---|---|
| CPT | 73721 | Magnetic resonance (eg, proton) imaging, any joint of lower extremity; without contrast material(s) |
| CPT | 20220 | Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma, bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types, trocar, or needle; superficial |
Medications:
Treatment requires a long course of high-dose intravenous antibiotics, such as
vancomycin
Vancomycin
Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear.
Glycopeptides or
piperacillin
Piperacillin
Semisynthetic, broad-spectrum, ampicillin derived ureidopenicillin antibiotic proposed for pseudomonas infections. It is also used in combination with other antibiotics.
Penicillins/
tazobactam
Tazobactam
A penicillanic acid and sulfone derivative and potent beta-lactamase inhibitor that enhances the activity of other anti-bacterial agents against beta-lactamase producing bacteria.
Cephalosporins, targeted to the specific pathogen identified by
bone
Bone
Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy.
Bones: Structure and Types culture.
| Coding System | Code | Description |
|---|---|---|
| RxNorm | 11124 | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides (ingredient) |
| RxNorm | 1148971 | Piperacillin Piperacillin Semisynthetic, broad-spectrum, ampicillin derived ureidopenicillin antibiotic proposed for pseudomonas infections. It is also used in combination with other antibiotics. Penicillins / Tazobactam Tazobactam A penicillanic acid and sulfone derivative and potent beta-lactamase inhibitor that enhances the activity of other anti-bacterial agents against beta-lactamase producing bacteria. Cephalosporins (ingredient) |