Nephritic syndrome is a broad category of glomerular diseases characterized by glomerular hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma, variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables loss of renal function, and hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension. These features are in contrast to those of nephrotic syndrome Nephrotic syndrome Nephrotic syndrome is characterized by severe proteinuria, hypoalbuminemia, and peripheral edema. In contrast, the nephritic syndromes present with hematuria, variable loss of renal function, and hypertension, although there is sometimes overlap of > 1 glomerular disease in the same individual. Nephrotic Syndrome, which includes glomerular diseases characterized by severe proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children, although there is sometimes overlap of > 1 glomerular disease in the same individual. The clinical presentations of nephritic syndrome are highly varied, from asymptomatic with urinary abnormalities to life-threatening critical illness. Diagnosis is suggested by hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma, mild-to-moderate proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children, and certain serologies (e.g., ANCA ANCA Group of systemic vasculitis with a strong association with anca. The disorders are characterized by necrotizing inflammation of small and medium size vessels, with little or no immune-complex deposits in vessel walls. Rapidly Progressive Glomerulonephritis); kidney biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is necessary in most cases. Management varies as widely as the clinical presentations, from watchful waiting in mild cases to immunosuppression and plasmapheresis Plasmapheresis Procedure whereby plasma is separated and extracted from anticoagulated whole blood and the red cells retransfused to the donor. Plasmapheresis is also employed for therapeutic use. Stevens-Johnson Syndrome in aggressive disease.
Last updated: Dec 15, 2025
Nephritic syndrome is defined by some or all of the following findings:
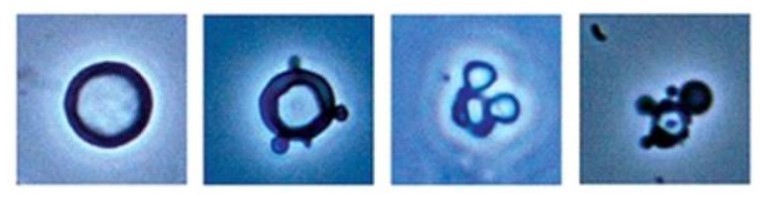
Urine microscopy of nephritic syndrome:
Left: normal RBC with circular appearance
Right (3 images): dysmorphic RBCs with blebs on the membranes and “Mickey Mouse” cells
The 2 main mechanisms of glomerular injury in the nephritic syndromes are immune complex–mediated and complement dysregulation. Hereditary forms of GN (e.g., Alport syndrome Alport Syndrome Alport syndrome, also called hereditary nephritis, is a genetic disorder caused by a mutation in the genes encoding for the alpha chains of type IV collagen, resulting in the production of abnormal type IV collagen strands. Patients present with glomerulonephritis, hypertension, edema, hematuria, and proteinuria, as well as with ocular and auditory findings. Alport Syndrome) have different pathophysiologies.
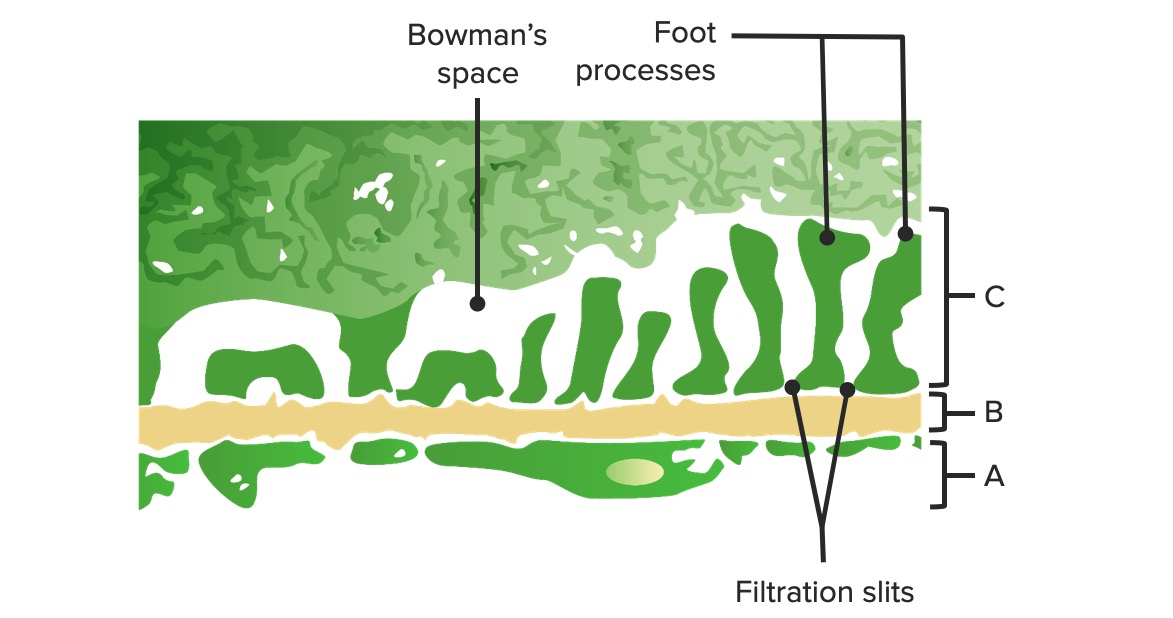
Diagram of the glomerular barrier:
A: Fenestrated endothelium of the glomerular capillaries
B: Basal membrane
C: Epithelial layer demonstrating podocyte foot processes and structural proteins creating the slit diaphragm
The primary and secondary causes of GN vary by etiology but have hematuria Hematuria Presence of blood in the urine. Renal Cell Carcinoma and variable Variable Variables represent information about something that can change. The design of the measurement scales, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Types of Variables degrees of proteinuria Proteinuria The presence of proteins in the urine, an indicator of kidney diseases. Nephrotic Syndrome in Children in common. Biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma findings differ and are important to know.
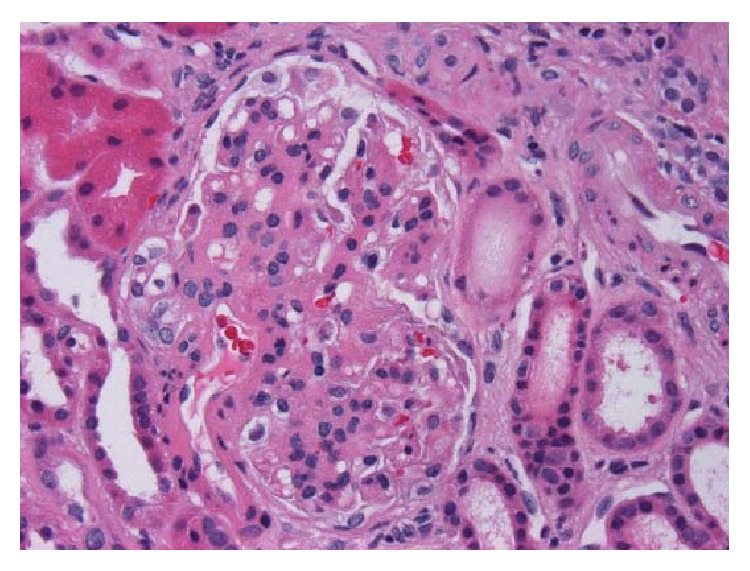
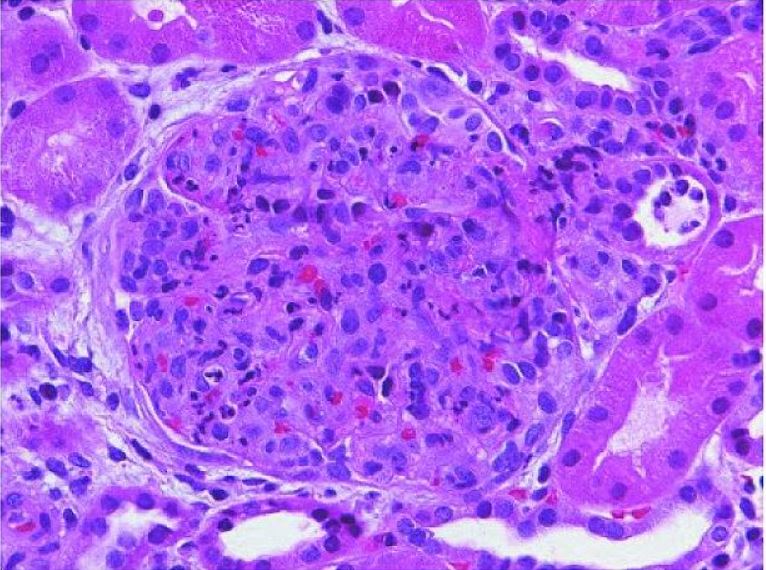
Kidney biopsy with IgA nephropathy:
H&E, x400. Glomerulus with thickened mesangium and segmental mesangial hypercellularity
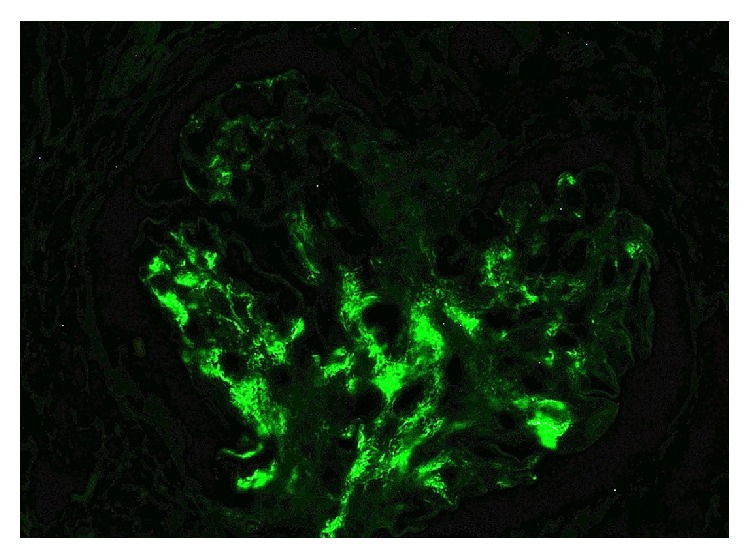
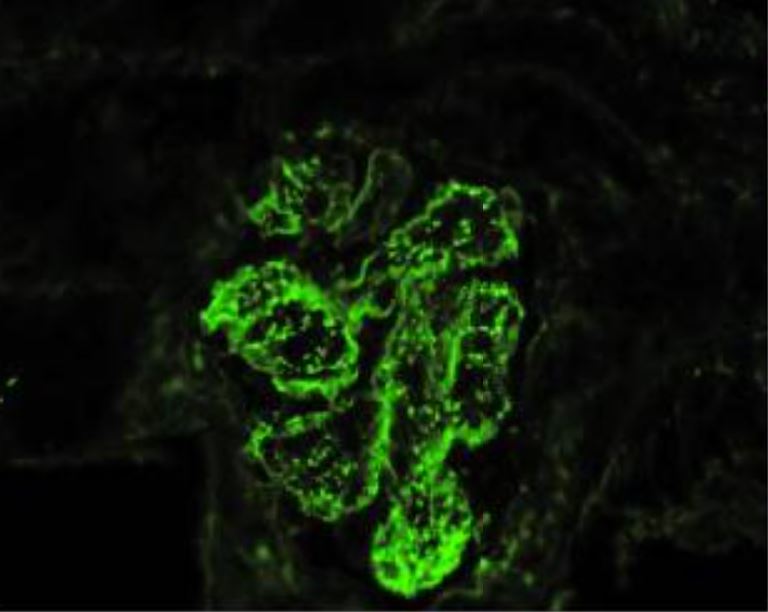
IgA nephropathy:
Immunofluorescence stain demonstrating positivity for IgA
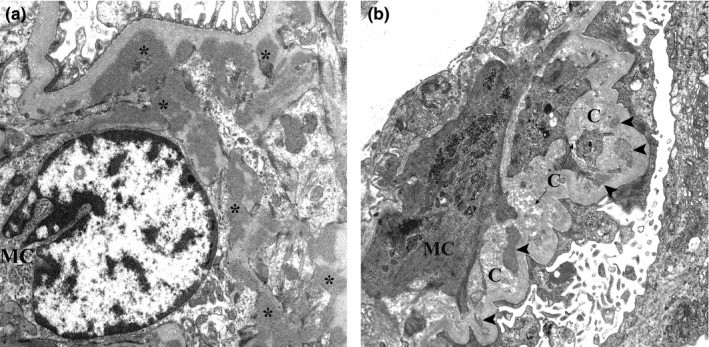
Electron micrograph of kidney biopsy of IgA nephropathy:
(a): Several electron-dense mesangial deposits (asterisks) are shown. These deposits lack the electron‐lucent halo.
(b): Mesangial deposits with varying degrees of resorption (arrowheads) close to collagen fibers are evident.
Acute poststreptococcal glomerulonephritis:
An enlarged glomerulus with global closure of the capillary lumina caused by endogeneous predominantly mesangial cell proliferation and infiltrating blood-borne monocytes and polymorphonuclear leukocytes (H&E staining).
IgA-dominant acute poststreptococcal glomerulonephritis with concomitant rheumatic fever (immunofluorescence microscopy):
shows granular mesangial and glomerular capillary wall immune deposits with a “starry-sky” pattern of IgA dominance
IgA-dominant acute poststreptococcal glomerulonephritis with concomitant rheumatic fever:
Discrete electron-dense subendothelial and subepithelial deposits detected using high magnification shows granular mesangial and glomerular capillary wall immune deposits with a “starry-sky” pattern of IgA dominance
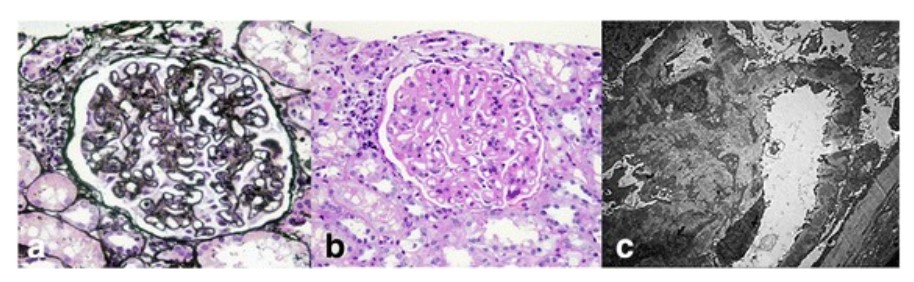
Renal histopathologic findings in systemic lupus erythematosus:
Light micrographs of a glomerulus show diffuse thickening of the glomerular basement membrane (periodic acid–silver methenamine stain; ×400) (a) with mesangial hypercellularity and mesangial matrix expansion (periodic acid–Schiff stain; ×400) (b). Electron microscopic analyses show numerous subepithelial and mesangial electron-dense deposits, as well as deposits within the glomerular basement membrane with extensive fusion of foot processes (×5000) (c).
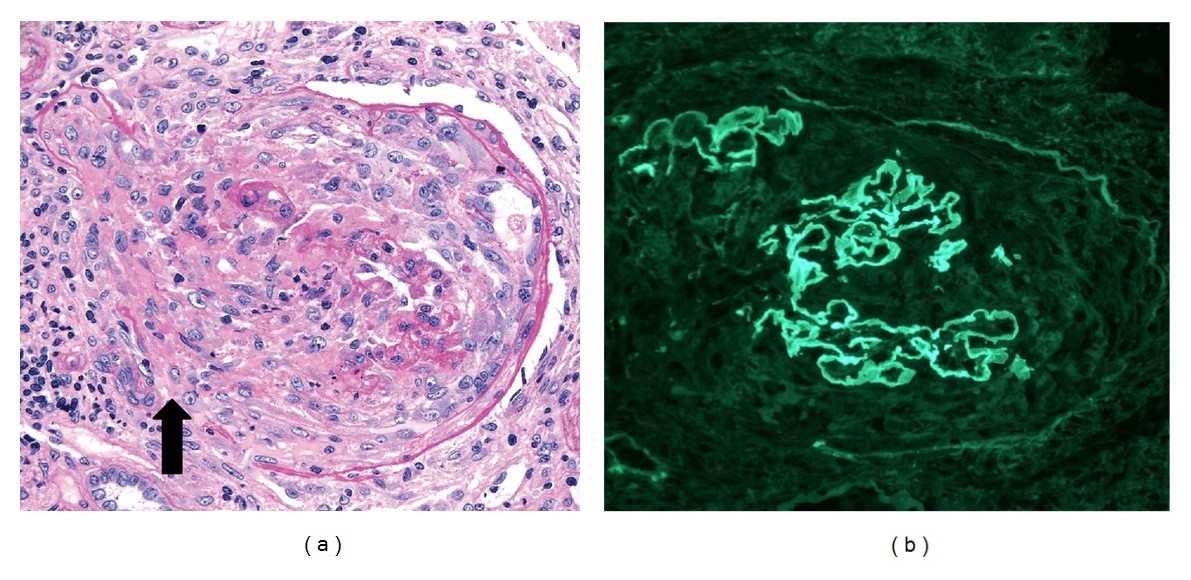
Glomeruli from a kidney biopsy of crescentic glomerulonephritis, with anti–glomerular basement membrane and p-ANCA antibodies:
(a): Light microscopy shows cellular destructive crescent with discontinuities in Bowman capsule (arrow; periodic acid–Schiff stain, ×250). Adjacent interstitium has a mononuclear leukocytic infiltrate.
(b) Immunofluorescence stain (×250) showing strong (3–4+) linear IgG staining along capillary walls. The capillary walls are disrupted focally because of crescent formation.
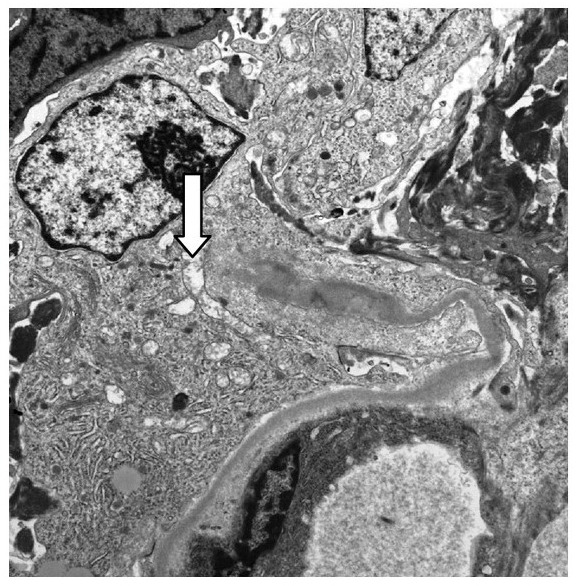
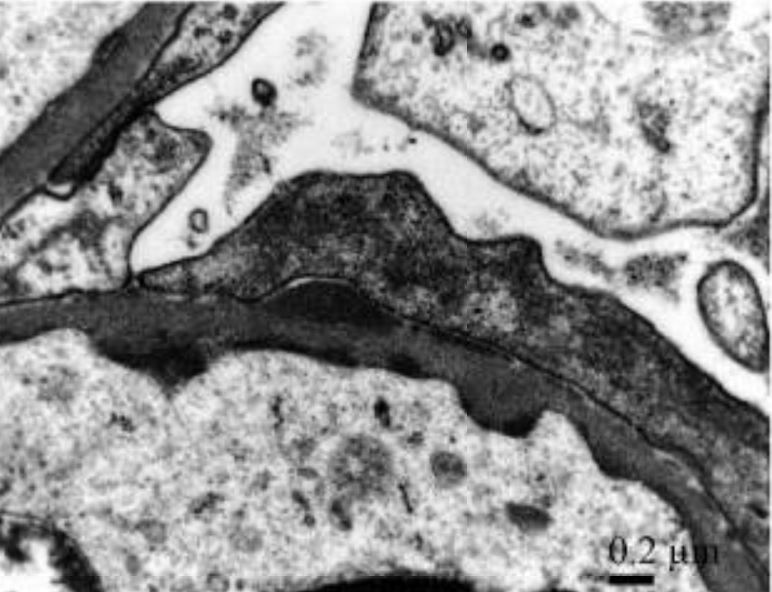
Electron micrograph ×10,000 showing a broken glomerular capillary wall (arrow) associated with a cellular crescent in Goodpasture disease
Image: “Glomeruli from the renal biopsy” by Tariq Javed and Parag Vohra. License: CC BY 3.0, cropped by Lecturio.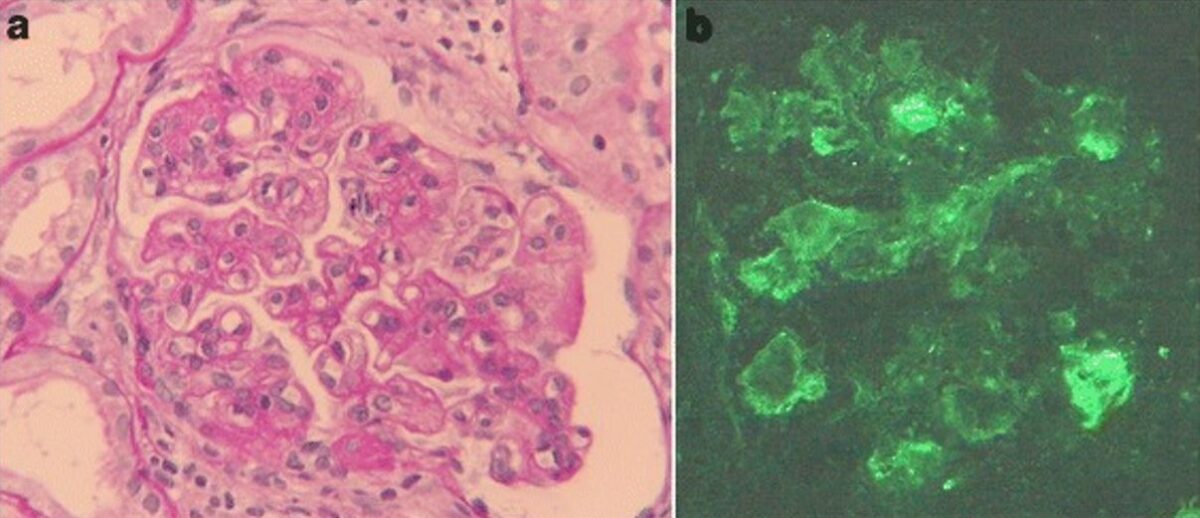
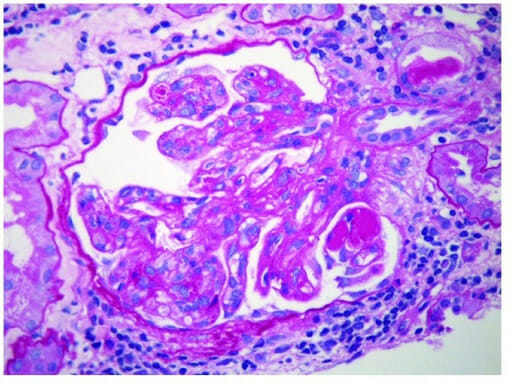
Membranoproliferative glomerulonephritis associated with hepatitis C
a) Light microscopy findings of kidney biopsy: Periodic acid-Schiff staining reveals mesangial hypercellularity, lobular accentuation, and double contour of the basement membrane (original magnification, ×400).
b) Immunofluorescence staining of IgM is positive along the capillary loop (original magnification, ×400).
Membranoproliferative glomerulonephritis:
Electron micrograph of MPGN showing subendothelial immune deposits