Myocarditis is an inflammatory disease of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy, which may occur alone or in association with a systemic process. There are numerous etiologies of myocarditis, but all lead to inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation and myocyte injury, most often leading to signs and symptoms of heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR). The course of myocarditis may vary based on the etiology and timeline of symptom progression. The diagnosis is supported by clinical findings, laboratory evaluation, and cardiac imaging. A definitive diagnosis by endomyocardial biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is rarely required. Management is supportive and aimed at addressing complications.
Last updated: Dec 15, 2025
Myocarditis is an inflammatory disease of the myocardium Myocardium The muscle tissue of the heart. It is composed of striated, involuntary muscle cells connected to form the contractile pump to generate blood flow. Heart: Anatomy.
The following table summarizes the infectious causes of myocarditis. Keep in mind that this list is not exhaustive.
| Viral | Bacterial | Parasitic | Fungal |
|---|---|---|---|
|
|
|
|
Inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation due to various etiologies leads to enlargement of the heart and dilation of all chambers.
The clinical presentation can vary based on the severity and temporal progression of symptoms. Most signs and symptoms are related to heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR).
Acute myocarditis: presentation and diagnosis within a short period of time (< 1 month)
Chronic myocarditis (chronic inflammatory cardiomyopathy Cardiomyopathy Cardiomyopathy refers to a group of myocardial diseases associated with structural changes of the heart muscles (myocardium) and impaired systolic and/or diastolic function in the absence of other heart disorders (coronary artery disease, hypertension, valvular disease, and congenital heart disease). Cardiomyopathy: Overview and Types): myocardial inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation with established dilated cardiomyopathy Dilated Cardiomyopathy Dilated cardiomyopathy (DCM) is the most common type of non-ischemic cardiomyopathy and a common cause of heart failure (HF). The cause may be idiopathic, familial, or secondary to a variety of underlying conditions. The disease is characterized by the enlargement of 1 or both ventricles and reduced systolic function. Dilated Cardiomyopathy generally > 1 month
Classic presentation:
Note: initial evaluation generally includes lab tests (CBC with differential, inflammatory and cardiac biomarkers, etc ETC The electron transport chain (ETC) sends electrons through a series of proteins, which generate an electrochemical proton gradient that produces energy in the form of adenosine triphosphate (ATP). Electron Transport Chain (ETC)), ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG), echocardiogram Echocardiogram Transposition of the Great Arteries, chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests. It is important to rule out obstructive coronary artery Coronary Artery Truncus Arteriosus disease in those at risk.
Pivotal tests for making the diagnosis of myocarditis are cardiac magnetic resonance Cardiac magnetic resonance Aortic Regurgitation ( CMR CMR Imaging of the Heart and Great Vessels) imaging (non-invasive) and endomyocardial biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma (invasive and not always performed).
Laboratory studies:
ECG ECG An electrocardiogram (ECG) is a graphic representation of the electrical activity of the heart plotted against time. Adhesive electrodes are affixed to the skin surface allowing measurement of cardiac impulses from many angles. The ECG provides 3-dimensional information about the conduction system of the heart, the myocardium, and other cardiac structures. Electrocardiogram (ECG):
Chest X-ray X-ray Penetrating electromagnetic radiation emitted when the inner orbital electrons of an atom are excited and release radiant energy. X-ray wavelengths range from 1 pm to 10 nm. Hard x-rays are the higher energy, shorter wavelength x-rays. Soft x-rays or grenz rays are less energetic and longer in wavelength. The short wavelength end of the x-ray spectrum overlaps the gamma rays wavelength range. The distinction between gamma rays and x-rays is based on their radiation source. Pulmonary Function Tests:
Echocardiogram Echocardiogram Transposition of the Great Arteries:
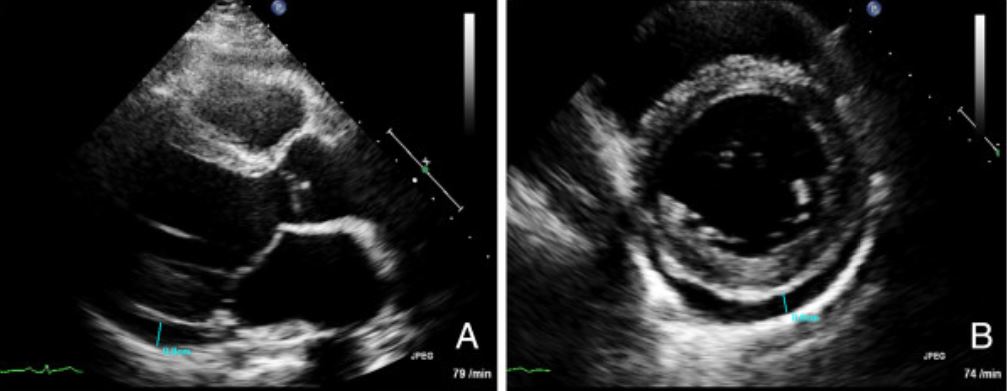
Transthoracic echocardiogram images for a patient with myocarditis:
(A) Long axis view and (B) short axis view demonstrating a pericardial effusion (marked in blue)
Cardiac MRI Cardiac MRI Imaging of the Heart and Great Vessels:
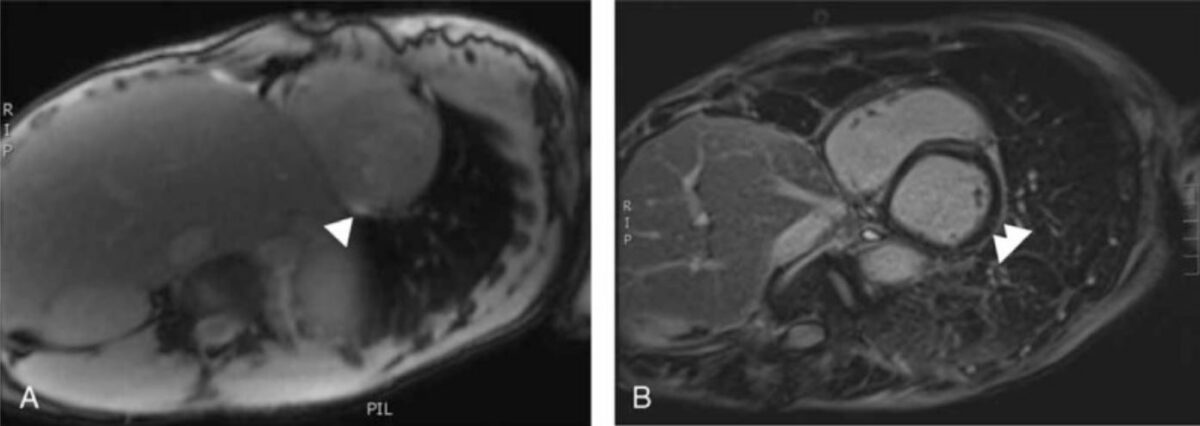
Cardiac MRI suggestive of myocarditis. White arrows mark enhancement of the myocardium, which is suggestive of edema
Image: “Myocarditis in Patients With Antisynthetase Syndrome: Prevalence, Presentation, and Outcomes” by Dieval, C. et al. License: CC BY 4.0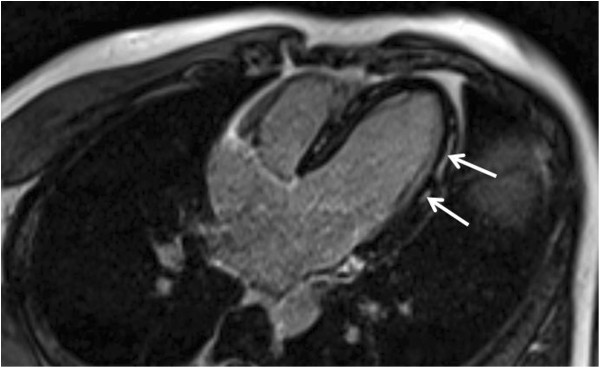
Cardiac MRI demonstrating mid-wall gadolinium enhancement of the lateral wall, which is a characteristic finding
Image: “Myopericarditis complicated by pulmonary embolism in an immunocompetent patient with acute cytomegalovirus infection: A case report” by Vandamme, Y.M. et al. License: CC BY 2.0Endomyocardial biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is the gold standard for diagnosis; however, it is rarely needed.
Indications:
Findings:
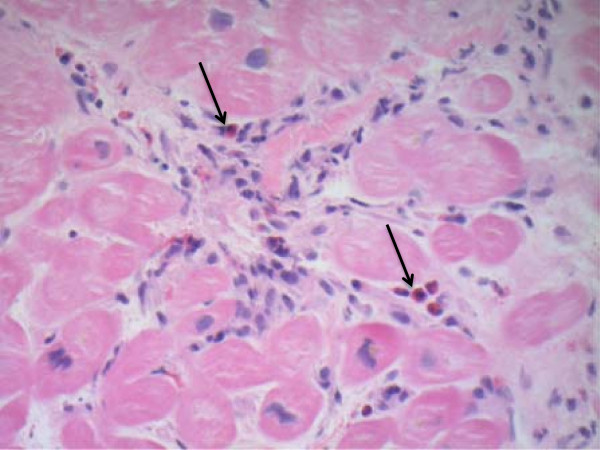
Endomyocardial biopsy in eosinophilic myocarditis:
There is infiltration of eosinophils (arrows) seen on hematoxylin and eosin staining.
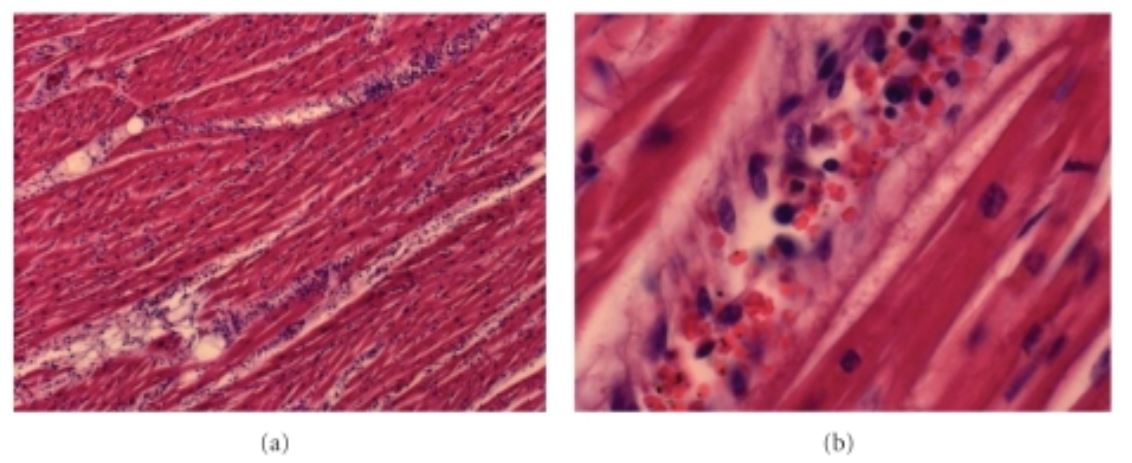
Acute myocarditis due to Plasmodium falciparum:
There is extensive lymphocytic infiltration.
Management for myocarditis is generally supportive, but often includes:
To aid in risk stratification, treatment decisions and monitoring of disease progression:
Medical therapy for heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR):
For fulminant heart failure Heart Failure A heterogeneous condition in which the heart is unable to pump out sufficient blood to meet the metabolic need of the body. Heart failure can be caused by structural defects, functional abnormalities (ventricular dysfunction), or a sudden overload beyond its capacity. Chronic heart failure is more common than acute heart failure which results from sudden insult to cardiac function, such as myocardial infarction. Total Anomalous Pulmonary Venous Return (TAPVR):
Most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship will have a partial or full recovery. However, long-term follow-up and monitoring are recommended.